Osteoporosis Treatment and Management
Osteoporosis translates to “porous bone.” If you have this illness, which weakens your bones, you are more likely to suffer from fractures in odd places, such as your wrists or hips. Reduced bone mass and strength are symptoms of osteoporosis. Rarely do people notice the condition’s onset until the weakening bones create a painful fracture? The hip, wrist, and spine account for most of these breaks. Osteoporosis treatment and management often entail behavioural modifications related to diet and activity, in addition to the medication that either decreases bone breakdown (also known as bone resorption) or enhances bone production.
Osteoporosis Treatment and Management
Osteoporosis is treated with various drugs to lower the risk of fractures. Most of these drugs either stop bone loss (in which case they are called antiresorptive drugs) or stimulate bone development. The only way to get these drugs is via a prescription from a medical professional.
Before starting osteoporosis medicine, make sure the doctor is aware of any other prescriptions you are taking or health concerns you have. After determining that a patient has osteoporosis or osteopenia with high fracture risk, medication may be administered. Medicines for osteoporosis help increase bone mass and protect against breaks.
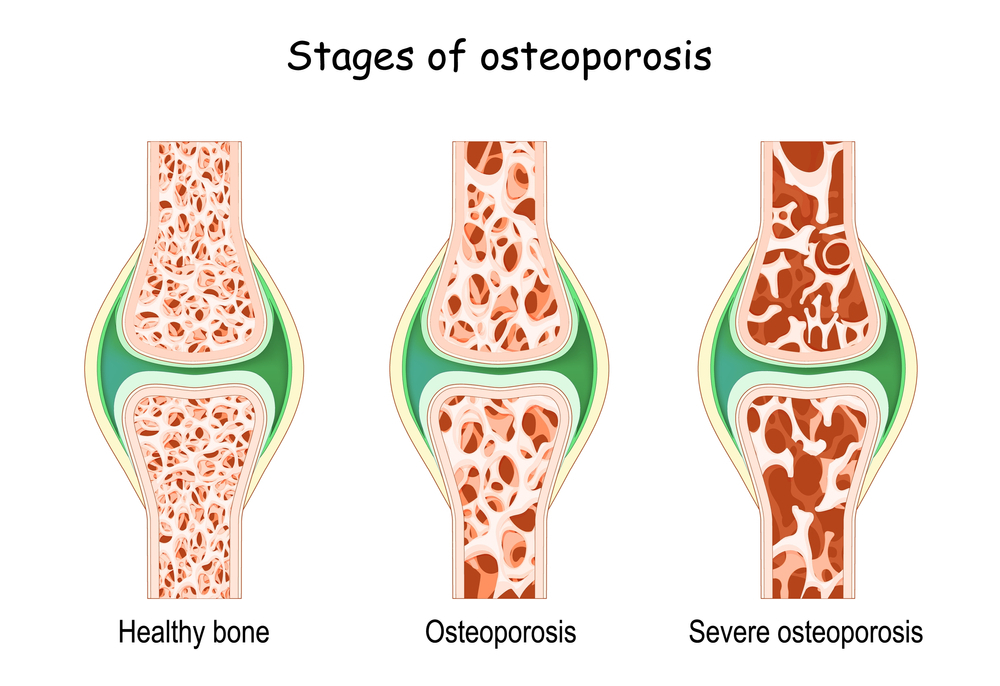
Osteoporosis stages
Osteoporosis medications can either promote bone growth or slow bone loss. Wear and tear on your bones may exceed your body’s capacity for repair as you age. Osteoporosis may be diagnosed if a significant bone loss occurs. Although there is currently no treatment for osteoporosis, its progression can be slowed or halted with medication and lifestyle changes.
Bisphosphonates for Osteoporosis
Osteoporosis treatment typically consists of bisphosphonates. Bone loss (anti-resorptive drugs) can be slowed with the help of bisphosphonates by inhibiting the activity of osteoclasts. These cells are responsible for absorbing calcium and facilitating the breakdown of bone cells.
Reducing the rate of bone loss helps prevent osteoporosis and lowers the risk of fractures in individuals who already have it. The Food and Drug Administration (FDA) has approved the following bisphosphonates for Osteoporosis treatment and management:
-
Alendronate
This aids in the treatment and prevention of bone loss after menopause. This drug also effectively treats secondary osteoporosis in men and women who use glucocorticoids and increases bone mass in males with osteoporosis. Daily or weekly oral administration of Alendronate is recommended.
-
Ibandronate
Only women who have gone through menopause and osteoporosis would benefit from this. Every month, you should take a pill orally. Once every three months, ibandronate can also be given intravenously.
-
Risedronate
Osteoporosis treatment and management are brought on by factors like menopause, low testosterone (hypogonadism), and extended steroid use. Patients of either sex and with several types of osteoporosis may take this drug orally, depending on individual needs. The typical dosing schedule for risedronate is administered orally once per day, once per week, or once per month.
-
Zoledronic Acid
Menopause, low testosterone levels, and steroid use can all lead to bone loss. Hence this is used to both prevent and treat osteoporosis. Once yearly, this drug is given via intravenous infusion.
Bisphosphonate supplements typically only show their worth in the first five years of use. To avoid side effects, including jaw bone death and atypical femur fractures, a medical professional should assess these medications every three to five years.
Denosumab for Osteoporosis
Denosumab (Prolia) blocks the bone-resorbing cells called osteoclasts, thereby slowing the bone-thinning process and boosting bone density. The most common applications of this drug are:
-
Addressing Osteoporosis After Menopause
Patients with osteoporosis who have not responded to or are intolerant of existing osteoporosis drugs can now receive effective treatment. Secondary osteoporosis due to breast and prostate cancer treatments can be treated by increasing bone mass in the patient.
Denosumab is an injectable medication that is administered once every six months. The injection can be given in the stomach, the thigh, or the upper arm. Denosumab may be best used with supplemental calcium and vitamin D for optimal bone health.
-
Estrogen/Hormone Replacement Therapy for Osteoporosis
Women who experience menopause prematurely or cannot handle other osteoporosis drugs may benefit from oestrogen replacement treatment to prevent excessive bone loss (anti-resorptive). Estrogen has a significant function in bone remodeling by preventing excessive bone loss.
The risk of osteoporosis can be postponed or reduced by increasing oestrogen levels, which may slow or prevent bone loss during the transition to menopause. Both oestrogen and progestin are options for hormone therapy. Some patients may avoid hormone replacement therapy that relies on oestrogen because of the risk of adverse effects, particularly cardiovascular side effects, including stroke and heart attack.
Anti-Thyroid and Anti-Parathyroid Hormone Treatment
Hormones usually secreted by the thyroid and parathyroid glands can affect bone formation mimicked by their synthetic analogs, calcitonin, abaloparatide, and teriparatide.
-
Teriparatide
This boosts bone mineral density not by reducing bone loss but by increasing the pace at which new bone is formed. Teriparatide treats osteoporosis in postmenopausal women, low testosterone in males, and long-term steroid use in both sexes. Self-injection of teriparatide into the thigh or abdomen once daily is safe and effective for up to 2 years of treatment.
-
Abaloparatide
This boosts the activity of bone-forming cells called osteoblasts, resulting in a faster rate of bone production. This medicine is prescribed to those with postmenopausal osteoporosis to boost bone density and strength and lessen the likelihood of fracture. Abaloparatide is administered intravenously (IV) once daily for up to two years.
-
Calcitonin
By stifling the activity of bone-resorbing osteoclasts, this treatment slows the deterioration of bone tissue. Women at least five years past menopause take this medicine because of its primary spinal effects. You can get your daily dose of calcitonin either by injecting it or through a nasal spray. As calcitonin’s effectiveness rises, the dosage required may be decreased.
Taking calcitonin for more than six months is not recommended. The reduced potency of calcitonin and teriparatide compared to bisphosphonates makes them attractive alternatives for people unable to take or choose not to take these harsher drugs.
Can Osteoporosis Medications Hurt Your Bones?
Occasionally, bisphosphonates and Denosumab can cause a fracture or crack in the thigh bone’s center. Pain in the thigh or groin is a common symptom of an atypical femoral fracture, which can develop slowly but steadily.
Rarely, bisphosphonates and Denosumab can lead to osteonecrosis of the jaw, which occurs when a piece of jawbone takes an unusually long time to heal or doesn’t heal after invasive dental procedures like tooth extraction. People with bone cancer, who take far higher doses of bisphosphonate than those generally used for osteoporosis, are more likely to experience this side effect.
Physiotherapy And Osteoporosis
If this condition isn’t properly diagnosed or treated, it can progress insidiously and show no outward signs until complications arise, such as a fracture. Osteoporosis preventive efforts should prioritize measures that increase bone density and lessen the chance of falls.
Physiotherapy is a vital aspect of the treatment for this medical condition. When done correctly and under the supervision of a trained specialist, specific workouts can help strengthen the bones. This article will focus on the management of osteoporosis with physiotherapy and the measures that should be taken to avoid complications associated with the condition. Physical therapists specialize in tailoring treatment plans for patients who have osteoporosis.
People with osteoporosis can’t follow a standard fitness program. Each patient’s program is customized based on medical data collected on the patient’s mobility, muscle strength, general fitness, fracture risk, stride, and balance. They tailor a plan to each person’s requirements.
Physiotherapy Management
- Bone-building and bone-loss-preventing exercises are age-agnostic and highly specialised.
- A physiotherapist may recommend a brace or other external device to help with posture and recovery.
- Uses a variety of techniques to alleviate suffering
- Range of motion (ROM) and strengthening exercises
Posture can be enhanced by mild range-of-motion and strengthening exercises prescribed by a physiotherapist. More bending at the thoracic spine means more fractures and vertebral wedging opportunities. A significant element of many different issues is having poor posture. Activities, light range of motion, and strength training will help you keep your upper back and core mobile and healthy.
-
Resistance Exercises
The risk of falling and breaking a bone can be reduced with the help of an exercise program designed by a physiotherapist. Exercise bands, gravity resistance exercises (such as squats, single-leg heel raises, and prone trunk extension with a cushion to protect the lowest ribs), push-ups, lunges, and sustained standing in a neutral spine posture are all part of a well-rounded exercise program.
-
Loading Exercises
Weightlifting and other low-impact exercises can reduce fracture risk by increasing overall stability and bone strength. People with osteoporosis often avoid weightlifting and other high-impact activities because of their disease. Exposure to a greater-than-usual load is necessary to strengthen any physiological system to increase its function.
Bones need to be subjected to forces beyond what they can handle daily to get stronger. It is feasible to lift heavy weights while keeping a healthy position and preventing harm to the back and legs. This can be accomplished by using proper form. Stomping, heel drops, dancing, and jogging are some weight-bearing activities done while being coached.
-
Balance And Coordination Exercises
Exercises that improve coordination and balance also aid in lowering the risk of falls. These routines help enhance equilibrium on uneven ground or for navigating tight places. Balance can be improved and checked with difficult exercises on both balls. Exercises are done twice or thrice weekly as part of a larger fitness plan.
What Is The Most Effective And Secure Therapy For Osteoporosis?
Everyone should know: what is the best and safest treatment for osteoporosis? Osteoporosis treatment and management typically begin with bisphosphonates. Medicines called bisphosphonates prevent bone from resorbing or reabsorbing quickly (i.e., resorption). In postmenopausal women, they are commonly used for both the prevention and treatment of osteoporosis.
Osteoporosis Symptoms
Breaking or fractured bones from minor trauma, such as falling, is the hallmark of osteoporosis. Additional osteoporosis symptoms include:
- Pain in the back and gradual reduction in height
- Stress fractures, which are microscopic breaks in the bone that might feel like muscle or joint discomfort
How To Treat Osteoporosis Without Medication
How to treat osteoporosis without medication? It’s possible to make a difference by staying active, eating a diet high in calcium and vitamin D, and avoiding falls. But these alone aren’t sufficient in every situation. This is why medical treatment may be recommended. Knowing the landscape of available osteoporosis medications is helpful. How to treat osteoporosis without drugs.
-
Diet and Nutrition
Patients with osteoporosis should get the calcium and vitamin D they need from a well-balanced diet. Every patient can benefit from learning from their doctor, nutritionist, or another health expert the recommended daily allowances for calcium and vitamin D, as well as simple strategies for including these nutrients in their diets.
-
Calcium
The initial recommendation for most patients is to improve their calcium intake via food. Patients with dairy allergies are often advised to take a supplement. Calcium can also be found in meals fortified with it and in dark leafy greens. Extra calcium intake, whether from food or supplements, is not encouraged. Problems like kidney stones, heart disease, and stroke may all be exacerbated by an excess of calcium.
-
Lifestyle Changes
Exercising can help you avoid falls by strengthening your muscles and bones. You can lower your risk of bone fracture by working with your doctor or physiotherapist to create a safe activity plan tailored to your requirements.
This is illustrated through activities such as weightlifting and various other types of strength training, as are other forms of weight-bearing exercise (exercises done while on your feet so that you carry your weight), such as fast walking, running, tennis, and volleyball. To reduce the likelihood of future falls, practicing balancing exercises can be helpful.
-
Vitamin D
There are not enough food sources of vitamin D, so you might consider taking a supplement. Patients with osteoporosis should take vitamin D supplements, but the exact dosage depends on their nutritional requirements. Vitamin D intakes beyond the typical daily recommendation of 15 mcg to 20 mcg are prevalent (800 IU). Daily doses of up to 100 mcg are deemed safe.
-
Exercise and Fitness
Bone density and general muscle strength can be maintained and improved via regular exercise, lowering the risk of falls. Strengthening muscles and weight-bearing movements are crucial for bone health and avoiding falls.
-
Reducing the Risk of Falling
Due to the weakened state of the bones caused by osteoporosis, it is essential that any potential for a high-impact injury, such as a fall, be avoided. T
Living With Osteoporosis Of The Spine
What is it like living with osteoporosis of the spine? The fragility of the bones in the spine makes osteoporosis a potential cause of short stature. This results in the spine being unable to support the body, leading to a stooped posture properly. Experiencing this pain is possible and can also develop into chronic discomfort.
The doctor or nurse at your clinic might be able to assist you. Patients with osteoporosis can expect to live for more than 15 years on average, and this is especially true for women under the age of 75 and men under the age of 60, underscoring the need for instruments for long-term care.
Conclusion
We have discussed a brief overview of the various aspects of osteoporosis treatment and management diagnosis, therapy, and medication. It doesn’t mean offering a replacement for professional medical advice but as a tool to aid in evaluating possible diagnoses and treatments.
All possible illnesses, treatments, drugs, side effects, and hazards that could affect a particular patient are NOT included. This data is not intended for a doctor’s examination and assessment of a patient’s situation, nor is it intended to be used in place of professional medical advice, diagnosis, or treatment.
Patients should consult the doctor if they have concerns about their health, symptoms, or treatment options (including any medications’ potential hazards and benefits). Nothing in the previous paragraphs should be construed as recommending that any particular treatment or medicine is appropriate for any patient’s needs.
How can you book an appointment?
We aim to see you within 24 hours so contact us to make an appointment either online at www.primphysiocare.co.uk or to find out more information on how we can help you, please call us on 07515280990 or email us primephysiocareluton@gmail.com. We are one of the best clinics whose physios are registered with HCPC, CSP and Physio first as well have enormous experience.
Google FAQs
How can I get the best results from osteoporosis treatment?
Treatment of Osteoporosis typically begins with bisphosphonates. These include Alendronate, a weekly tablet. Take one pill of risedronate (Actonel) once every two weeks or monthly.
What are the three methods of osteoporosis treatment and prevention?
Alendronate, Ibandronate, Risedronate, Zoledronic acid.
Treatments for osteoporosis typically include what?
Bisphosphonates are drugs that inhibit the body’s natural bone-resorbing enzymes (i.e., resorption). They are commonly given to postmenopausal women to prevent and treat the onset of osteoporosis.
How do you deal with osteoporosis?
If you want strong bones, there are steps you can take at any age. Getting enough calcium and vitamin D by eating the right foods is crucial. So does frequent weight-bearing activity, such as weight training, hiking, jogging, tennis, and dancing.
What is the severity of spinal osteoporosis?
Weakened vertebrae in the spine might collapse, leading to back pain, shorter stature, and a stooped posture. Osteoporosis Is most significant side effect is a fracture, especially in the hip or spine.
Can osteoporosis be treated with physical therapy?
A physiotherapy is an evidence-based option for the treatment and management of osteoporosis. It helps with pain management, enhances balance and posture, and fortifies muscles and skeleton. Lifting weights and lower impact exercises can lessen the chance of fracture by boosting bone strength.
What foods fight osteoporosis?
Vegetables with dark green leaves include kale, spinach, turnip greens, and brussels sprouts. Certain brands of drinks, breakfast meals, soy milk, snacks, and bread may contain added calcium and vitamin D.