Osteoporosis: 5 Proven Steps to Prevent Osteoporosis Fractures
Osteoporosis
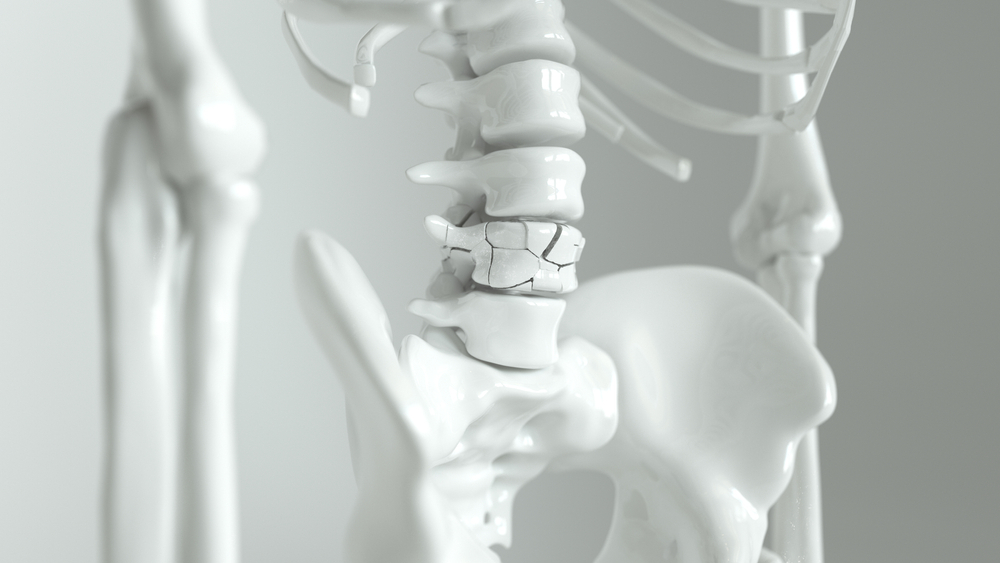
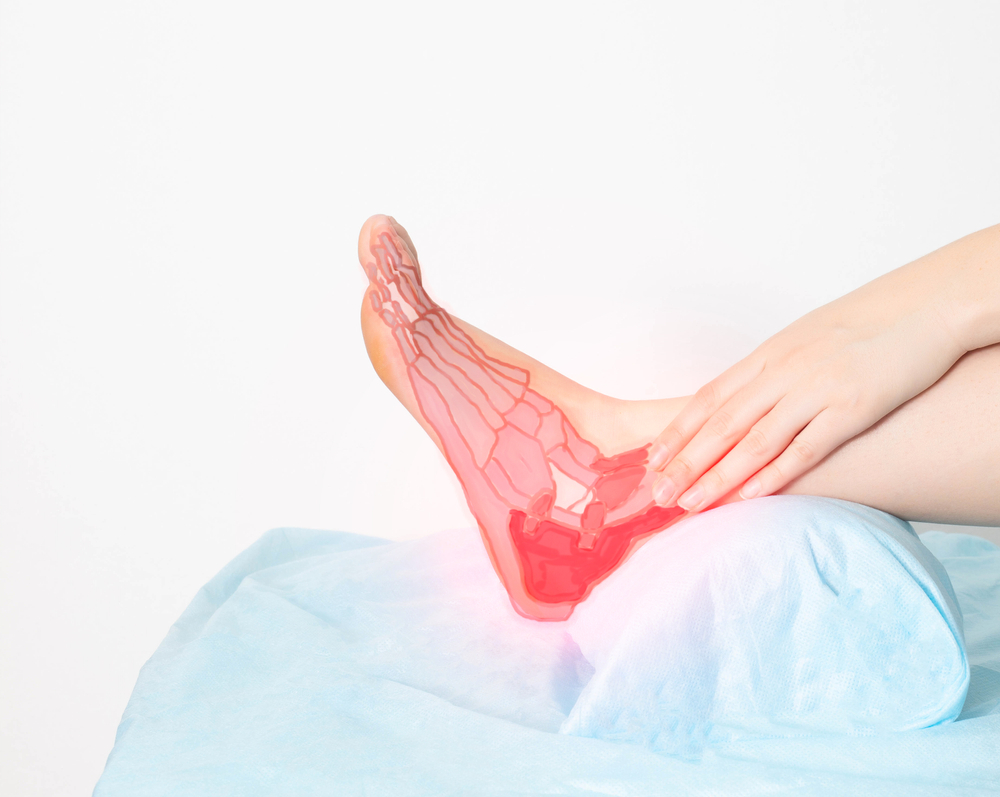
Osteoporosis is a condition that weakens bones to the point where they shatter easily, most frequently the hip, wrist, and backbone. Because you might not notice any changes until a bone breaks, osteoporosis is a “silent illness.” But over time, the strength of your bones has been deteriorating. An older woman performing resistance training. Here you can find 5 proven steps to prevent osteoporosis fractures.
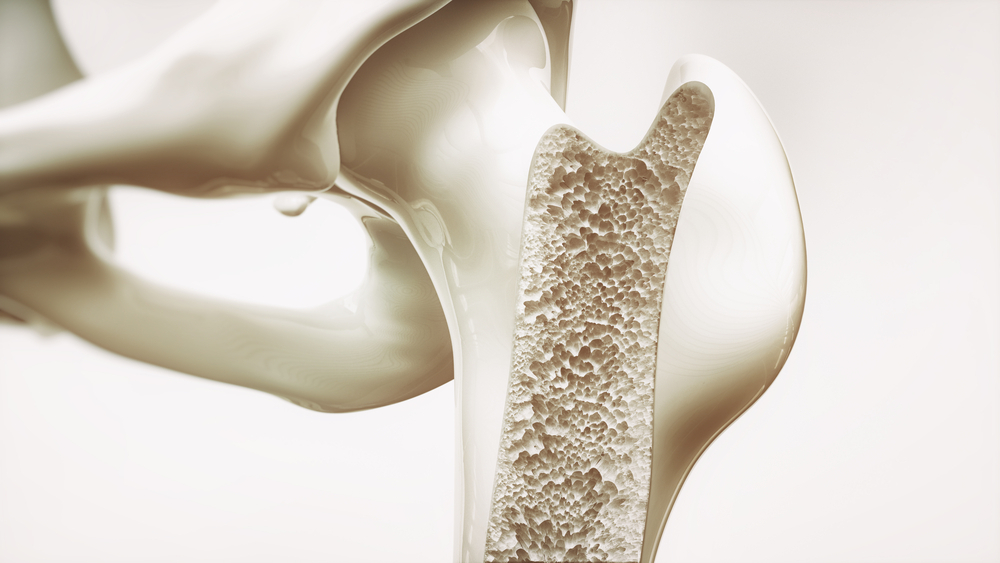
Bone is a living substance. The objective for bone health is to preserve as much bone as possible for as long as possible after the age of 30, when bone mass stops expanding. More bone loss than bone gain may occur as adults reach their 40s and 50s.
A honeycomb-like structure can be seen when closely examining the inside of a bone. The honeycomb’s gaps enlarge with osteoporosis, while the bone that makes up the honeycomb shrinks. Your bones’ exterior layer also becomes progressively thinner.
5 Ways To Prevent Osteoporosis Fractures
According to a study, the 5 below proven steps prevent osteoporosis fractures. Many people have broken a bone in a fall at some point in their life or know someone who has. Therefore, we know how simple it is to fracture a bone. Accidents occur frequently, and when they cause a bone fracture, the road to recovery can be challenging. A trip to an orthopaedic physician and perhaps even surgery may be necessary. Besides, after the cast is removed, these injuries frequently need extra care, such as physical therapy.
Without a doubt, preventing bone fractures is crucial for various reasons, regardless of an individual’s age. On the other hand, bone fractures develop into more serious conditions as people age and are also more prone to occur. A hip fracture, for instance, can result in major health issues and hip fracture rates rise exponentially with age. The American Academy of Orthopaedic Surgeons states that fragility fractures are the main reason for hospitalisation or death in persons 65 and older.
-
Exercise
Exercise that involves lifting weights promotes bone density and enhances balance, which helps prevent falls. Established osteoporosis is not treated by it. Before beginning a new fitness regimen, speak with your doctor, especially if you’ve been inactive, are older than 75, or have a health issue.
-
Calcium-Rich Diet
Building and keeping strong, healthy bones depends on consuming a nutritious, balanced diet that includes a range of foods and an adequate amount of calcium. A key strategy of an osteoporosis plan for maintaining bone density is ensuring your diet has enough calcium.
Physical Therapy for Osteoporosis
Osteoporosis is a chronic disorder marked by a loss of bone mass and density, which increases the risk of fractures. Anyone can develop osteoporosis, and as people get older, their risk rises. The National Institutes of Health (NIH) states that if the disorder runs in your family, you have a higher chance of developing it. Medication, dietary and lifestyle changes, and physical therapy are typically part of the treatment plan.
Osteoporosis can be prevented and managed with physical therapy, often known as physiotherapy. A physical therapist designs a special workout regimen to build your bones and muscles over several weeks and months. Your balance will be improved, and your risk of falling will be reduced. Additionally, physical therapy can enhance your quality of life if you’re in chronic pain and aid in the recovery from an osteoporosis-related injury. We’ll provide an outline of physical therapy’s operation, the kinds of exercises that are frequently employed, their advantages, and more.
Osteoporosis Plan
There are 5 ways to prevent osteoporosis. You may do this at any age to prevent osteoporosis. It’s crucial to consume meals high in vitamin D and calcium. In the same way, routine weight-bearing exercises, including lifting weights, walking, trekking, jogging, climbing stairs, tennis, and dancing, are beneficial.
Osteoporosis Monitoring
Regular osteoporosis monitoring and follow-up are crucial parts of any osteoporosis treatment strategy to assess its effectiveness and make corrections. It is advised to have regular doctor checks as well as additional bone density testing. Some recommendations for monitoring osteoporosis treatment call for bone mineral density (BMD) measures.
Since treatment-induced changes in bone density may take up to 3 years to discover and do not indicate whether a fracture will occur, there isn’t enough evidence to back up this strategy. Although biochemical markers of bone turnover have the potential to be monitored because they adapt quickly to treatment and are more accurate predictors of fracture reduction, the unpredictability of their assessment diminishes their relevance in clinical settings. There is no evidence that either strategy increases therapy adherence.
Contrarily, there is proof that speaking with a healthcare expert promotes treatment compliance, regardless of comments on monitoring tests’ efficacy. Although there is currently no justification for the use of markers for bone turnover or bone density in routine monitoring, patients should be given all the information they need to make an informed decision about their care and be given a chance to speak with a healthcare provider about any concerns they may have.
Risk Factors For Osteoporosis
Osteoporosis can affect persons of any age, although it most frequently affects older adults, particularly older women. This illness affects men as well. Women of colour and Asian descent are especially susceptible to osteoporosis. Age increases your risk of developing osteoporosis. Women may experience rapid bone loss during menopause for several years. Following that, the loss slows down but keeps going. Men lose bone mass more slowly than women do. However, at 65 or 70, both sexes lose bone at the same pace. Osteoporosis risk factors include:
-
Advanced Age
Ages 65 and older are particularly at risk.
-
Gender
Due to menopause, women are at a far higher risk of bone loss than men. Men, who account for 20% of osteoporosis patients, are in danger.
-
Family And Personal History
This includes a history of bone fractures on the mother’s side of the family, an individual history of any bone fracture as an adult, and a family history of osteoporosis (after age 50).
-
Race
Women of colour and Asian women are more vulnerable.
-
Body Type
Women with tiny bones and weights under 127 pounds are more in danger.
-
Menstrual History And Menopause
An individual woman’s risk of osteoporosis increases with normal menopause. The risk is even higher if a woman experiences early menopause or stops menstruating before menopause.
-
Hypogonadism
Males with this illness are also said to have low levels of testosterone.
-
Lifestyle
Lifestyle factors that increase the threat of osteoporosis include a lack of calcium and vitamin D, insufficient exercise, particularly weight-bearing, alcohol consumption, and cigarette smoking.
-
Chronic Diseases
Certain drugs can weaken bones and cause “secondary osteoporosis,” as the term is known. According to estimates, 30% and 60% of males and nearly 50% of premenopausal women with osteoporosis have this disease. Additionally, secondary osteoporosis can result in additional bone loss in older men and postmenopausal women with primary osteoporosis.
This group includes certain drugs used to treat endocrine problems. In particular, the oral version of these drugs (at greater doses and for longer periods) can be particularly detrimental to bone health when used to treat disorders. It is not advised to change or stop taking these medications unless under a doctor’s supervision due to the diseases these medications are prescribed to treat.
-
Fall Proof Your Home
As we age, our vision starts to fail us, which might result in falls. Keep your home well-lit to improve your vision and reduce the likelihood of falling. Keep areas clear of items that could cause you to trip, lay down runners or carpets to cover slick surfaces, add handrails where necessary, and use a rubber mat in the shower or bathtub to prevent slips.
-
Medications
Due to side effects impairing your balance, some drugs can increase your risk of falling.
What Are the Personal And Lifestyle Factors That Increase the Risk of Osteoporosis?
Do you know the individual and lifestyle risk factors for osteoporosis? The following list includes both personal and behavioural risk factors for osteoporosis.
- Women over 50, of both white and Asian descent. Osteoporosis can affect men and women of any ethnicity, but Asian and white postmenopausal women are more at risk.
- Men with low levels of testosterone. Testosterone contributes to strong bones.
- Alcohol drinkers and smokers (more than two drinks a day on most days).
- Anyone is weighing under 125 pounds. Petite adults have smaller frames and lower peak bone mass; any bone loss with ageing is, therefore, more likely to result in a lower-than-average bone mineral density.
- Folks who have had bariatric surgery.
- Anyone who has a senior parent who had a hip fracture.
- Those suffering from an eating disorder, rheumatoid arthritis, inflammatory bowel illness, kidney disease, or liver disease.
- Daily users of oral corticosteroids or other high-risk medications (e.g., thyroid hormone replacement, immunosuppressant drugs, warfarin).
How To Prevent Osteoporosis After Menopause
Are you wondering about how to prevent osteoporosis after menopause? You may believe you are not at risk for bone loss because you feel fine. There shouldn’t be any concerns if there are no aches or fractures in the joints. Actually, no. Osteoporosis does not show symptoms until a bone is broken. Your doctor will ask about your family history, bone density, and hormone levels because you need to be extremely careful in this regard.
Alternatively, state the obvious: You should talk to your doctor about preventing osteopenia and osteoporosis if you are approaching menopause or are already exhibiting symptoms. You’ll feel the benefits in your bones! By implementing a few lifestyle suggestions, such as the following around menopause, you can lower your risk of acquiring osteoporosis:
- Attempt to consume 1,300 mg of calcium daily through your food. This is equivalent to three to four servings of dairy products. Numerous non-dairy foods also contain calcium, including dark green leafy vegetables, firm tofu, almonds, brazil nuts, unhulled tahini, and fish with edible bones, including sardines or canned salmon.
- Engage in regular weight-bearing exercises, such as resistance training with weights (always do this exercise under supervision).
- Keep your vitamin D levels healthy. The body can better absorb calcium with vitamin D. It is produced in the skin after sun exposure and is present in some foods in very minute amounts. A quick blood test can determine the vitamin D levels in the body.
- Avoid consuming alcohol in itself.
- Try not to smoke (smoking cigarettes is associated with a higher risk of osteoporosis).
- Avoid consuming too much caffeine.
These lifestyle behaviours should be established as early as possible for maximum advantage.
Osteoporosis Prevention
Osteoporosis is defined as “bones with holes.” Bones lose calcium and other minerals more quickly than the body can replenish them. They weaken, lose density, and break more easily. Since there are typically no warning signs or symptoms, most people don’t realize they have osteoporosis until a fracture occurs.
Because of this, osteoporosis is sometimes referred to as the “silent illness”. Although some males are also affected, osteoporosis is most common in middle-aged and older women. Changes in lifestyle and medical care can stop additional bone loss and lower your risk of bone fractures if you have osteoporosis. The 5 proven steps prevent osteoporosis fractures.
Osteoporosis Treatment
Treatment suggestions are frequently made using data from tests like the bone density test to assess your risk of breaking a bone in the next ten years.
-
Bisphosphonates
The most frequently recommended osteoporosis drugs are bisphosphonates, given to men and women at higher risk of fracture. There are several examples, such as Alendronate, Ibandronate, and Risedronate.
-
Alkyl zoledronate
Consequences include nausea, pain in the abdomen, and symptoms like heartburn. These are less likely if the medication is taken as directed. Although they don’t irritate the stomach, intravenous bisphosphonates can result in fever, headaches, and muscle aches.
The centre of the thigh bone breaking or cracking is a fairly uncommon side effect of bisphosphonates. Delay in the jawbone’s recovery is a second uncommon consequence (osteonecrosis of the jaw). This can happen when a tooth is extracted, or another invasive dental procedure is performed.
-
Denosumab
When compared to bisphosphonates, denosumab (Prolia, Xgeva) increases bone density and lowers the risk of all types of fractures. A shot under the skin is used every six months to provide denosumab.
Denosumab causes the same uncommon side effects as bisphosphonates, including jaw osteonecrosis and breaks or fissures in the centre of the thigh bone. Denosumab may need to be taken indefinitely if it is prescribed to you. According to recent studies, there may be a significant risk of spinal column fractures upon drug discontinuation.
-
Hormone-Related Therapy
Estrogen can support bone density maintenance, particularly when started soon after menopause. But oestrogen medication can also raise the risk of stroke-causing blood clots and breast cancer. As a result, oestrogen is primarily utilized to treat menopausal symptoms in younger women who need it for bone health.
Raloxifene imitates estrogen’s favourable effects on bone density in postmenopausal women while avoiding some dangers. Some kinds of breast cancer can be prevented by using this medication. One potential adverse effect is hot flushes. Your risk of blood clots may also be increased with raloxifene.
An age-related reduction in testosterone levels may be associated with osteoporosis in men. While testosterone replacement therapy can help with low testosterone symptoms, osteoporosis drugs are advised instead of or in addition to testosterone as they have been more thoroughly examined in male patients with the disease.
-
Bone-Building Medications
Your doctor may advise attempting the following if you have severe osteoporosis or if the more popular therapies for the condition don’t sufficiently relieve your symptoms:
-
Teriparatide
Like parathyroid hormone, this potent medication promotes the creation of new bones. For up to two years, it is administered by daily subcutaneous injection.
-
Abaloparatide
This medication shares similarity with parathyroid hormone. Only two years can be spent on this medication.
-
Romosozumab
This is the most recent osteoporosis drug that helps build bone. It is administered monthly at your doctor’s office and has a one-year treatment window.
You will typically need to take another osteoporosis treatment after stopping any of these bone-building medications to sustain the new bone growth. The 5 proven steps prevent osteoporosis fractures.
How can you book an appointment?
We aim to see you within 24 hours so contact us to make an appointment either online at www.primphysiocare.co.uk or to find out more information on how we can help you, please call us on 07515280990 or email us primephysiocareluton@gmail.com. We are one of the best clinics whose physios are registered with HCPC, CSP and Physio first as well have enormous experience.
Frequently Asked Questions
Q. How many fractures caused by osteoporosis can be avoided?
Ans. You can reduce your risk of developing many fractures by avoiding falls, keeping active, and consuming the correct vitamins and minerals. You can keep upright both indoors and outside by following some advice. Indoors: Balance: If you feel out of balance, think about balance training and physical treatment.
Q. What safeguards are necessary to stop the fracture from progressing?
Ans. These safety measures must be followed to stop the fracture from progressing.
- Healthy eating
- By eating well, you can keep your bones strong.
- Consider your health
What are three things you can take to ward off osteoporosis?
Ans. Here are three actions you may do to lessen your risk of osteoporosis:
- Recognize your hazards
- The first step to osteoporosis prevention is being aware of your dangers.
- Taking care of a fracture’s underlying cause
- Ensure that you receive an osteoporosis diagnosis and treatment if you have a fracture.
- Exercise Walking is a weight-bearing exercise that is particularly beneficial for the health of your bones.
Q.What Is Osteoporosis 2022’s Best and Safest Treatment?
Ans.The first line of treatment for osteoporosis is often composed of bisphosphonates. Denosumab is another popular osteoporosis drug. It might be utilized by individuals who cannot take bisphosphonates, such as persons with impaired renal function.