Who Is at Risk for Osteoporosis?
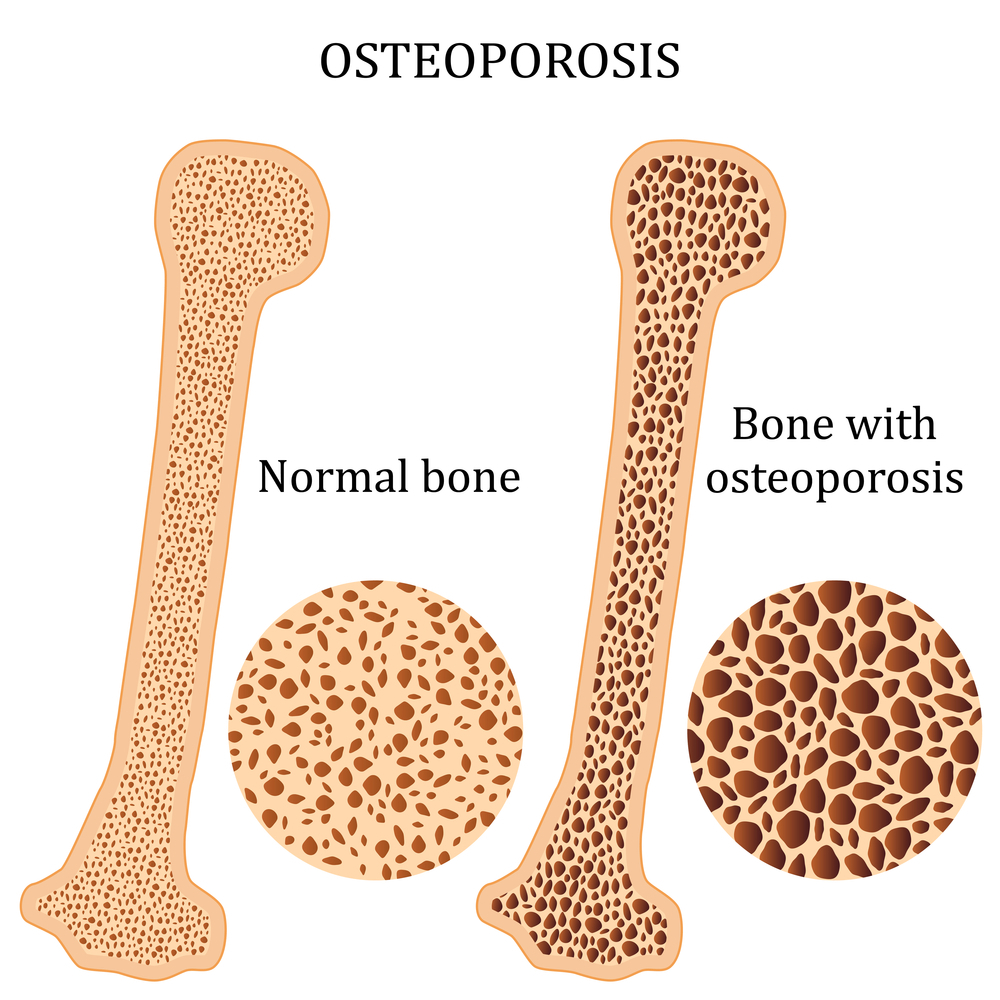
Ever wondered: who is at risk for osteoporosis? Because osteoporosis weakens bone tissue, people with the disease are at increased risk of fractures. Hip, wrist, and spinal fractures are the most common osteoporosis-related fractures. As living tissue, bone undergoes a continual process of breakdown and replacement. The disease osteoporosis develops when a bone is lost faster than you can replace it.
Osteoporosis strikes people of all ethnicities and sexes. Women of colour, particularly those white or Asian and past menopause, are at an increased risk. Bone loss and bone weakness can be avoided or reversed with the help of medication, a good diet, and weight-bearing activity.
What Is the Main Cause of Osteoporosis?
What is the main cause of osteoporosis? Your skeleton is constantly regenerating itself by forming new and destroying old bones. Bone mass rises as a young person because bone formation exceeds bone resorption. This process slows after the early 20s, and by the time most people reach their 30s, they have reached their maximum bone mass. People lose bone mass at a greater rate as they age than it is being replaced.
You must know: who is at risk for osteoporosis? Your risk of osteoporosis in later life is partially determined by how much bone mass you obtained when you were younger. Inheritance and racial background both play a role in determining peak bone mass. The greater your peak bone mass, the less probable you will have osteoporosis as you get older since you will have more bone “in the bank.”
10 Risk Factors for Osteoporosis
After learning who is at risk for osteoporosis?, you must know about the causes of osteoporosis. There are many potential causes, but age and gender are the two most important of the 10 risk factors for osteoporosis.
-
Age
The risk of fracture due to osteoporosis rises with age in both sexes. However, postmenopausal women over 50 are at greater risk of osteoporosis. Because estrogen production diminishes during menopause, women experience rapid bone loss throughout the first decade following menopause.
The effects of ageing and osteoporosis do not only affect women. Men over 50 have a higher risk of bone fractures due to osteoporosis than developing prostate cancer, which may surprise you. It is estimated that around 80,000 men will break their hips each year and that males have a higher mortality rate than women following a hip fracture.
-
Genetic Predisposition to Low Bone Density
To a large extent, genetics govern when a person reaches peak bone mass, which occurs between the ages of 18 and 25. The ability of the body to absorb vitamin D, in particular, is strongly influenced by a person’s genetic makeup. Reduced vitamin D reception has been linked to impaired bone formation and an increased risk of osteoporosis.
-
Ethnicity
Ethnicity also plays a role in determining your osteoporosis risk. Osteoporosis is more common in women of Asian and Caucasian descent. African American and Hispanic women, however, remain vulnerable. Regarding hip fractures, African American women have a higher mortality rate than white women.
-
Gender
Women are more likely to experience a fracture because their bones are more delicate, and their bone mass is smaller than men’s. The disease most commonly affects postmenopausal women. Women tend to live longer than males, and their lighter, more brittle bones contribute. Osteoporosis is more common in women, although men can have it too.
-
Body Weight
Body fat percentage and bone density are other important factors. Due to the greater risk of bone loss, people of smaller stature are more likely to suffer from osteoporosis.
-
Menopause
Lowered estrogen levels during menopause disrupt the bone remodelling process and increase the rate of bone loss, leading to weaker bones and an increased risk of fracture.
-
Menstrual History in Females
Having light periods for most of your life and experiencing menopause at a younger age can put you at a slightly increased risk for osteoporosis.
-
Low Testosterone in Males
Lower than normal testosterone levels in men have been linked to a higher risk of osteoporosis and impaired bone development.
-
Family History
Having a loved one with osteoporosis is a major risk factor for developing the condition oneself. You might be at a higher risk of osteoporosis if your parents or grandparents experienced disease symptoms, such as a fractured hip following a relatively minor fall.
-
Medications
Certain diseases and drugs heighten the danger. Some of the following disorders are linked to erratic hormone levels, so you and your doctor may want to explore osteoporosis screening early if you have or have ever had one of these conditions.
- The adrenals, thyroid, or parathyroid glands are overworking.
- Transplantation or weight loss surgery (bariatric) background.
- Lack of periods or hormone therapy for breast or prostate cancer.
- Gluten intolerance is often known as inflammatory bowel disease.
- Illnesses of the blood, such as multiple myeloma.
Bone loss and osteoporosis are possible negative side effects of some drugs. Steroids, drugs used to combat cancer, and medicines to control seizures are all in this category. Talk to your doctor about how your drugs may affect your bones.
All potential dangers may stem from external sources, but this is not necessarily the case. Some of the risk factors for osteoporosis are within your control. You should consult your doctor regarding any pharmaceutical concerns. Furthermore, you are accountable for your:
- Dietary insufficiency of calcium and vitamin D increases susceptibility to osteoporosis. Eating disorders like bulimia and anorexia can be prevented and treated.
- Sedentary (inactive) lifestyles are associated with an increased risk of osteoporosis.
- Use of tobacco products: smokers have a higher rate of bone fractures.
- The risk of developing osteoporosis is greatly exacerbated by alcohol consumption. Avoid alcohol.
What Are 5 Symptoms of Osteoporosis?
Do you know: what are 5 symptoms of osteoporosis? Common osteoporosis warning symptoms include:
-
Fragility-Related Fractures
Fractures of the wrist, back, hip, or other bones can result from a relatively minor collision.
-
Height Loss
Possible height loss due to ageing exceeding two inches.
-
Receding Gums
Gum recession occurs when the jawbone recedes, exposing more of the tooth root.
-
Curved Stooped Shape to the Spine
Vertebrae weakened by osteoporosis progressively assume a wedge form, causing the upper back to bend forward. This is generally referred to as a “widow’s hump.”
-
Lower Back Pain
Although osteoporosis doesn’t directly cause back pain, it does weaken the spine to the point that it can’t withstand everyday pressure.
Treatment for Osteoporosis
Medicines that strengthen bones are used in the treatment for osteoporosis, along with measures to treat and prevent fractures. Although your bone density scan is used to diagnose osteoporosis, it is not used to determine the course of treatment.
Osteoporosis can be treated with a wide variety of pharmaceuticals. In consultation with your doctor, you can find the optimal solution. In reality, it is impossible to identify a single optimal medicine for the treatment of osteoporosis. A cure is considered “best” if it is effective for the patient.
-
Physiotherapy Treatment
Physiotherapy, another name for physical therapy, can aid in treating and controlling osteoporosis. Over several weeks or months, your physical therapist will design a unique training plan to help you regain bone and muscle strength. You’ll have better stability and less risk of falling if you do this. Injuries sustained as a result of osteoporosis can be rehabilitated by physical therapy, and people living with chronic pain can also benefit greatly from this treatment.
Physiotherapy has been demonstrated to be useful in managing and treating osteoporosis. It helps with pain management techniques, enhances balance and posture, and fortifies muscles and skeleton. Increasing bone strength through weightlifting and low-impact exercise can reduce fracture risk.
-
Hormone and Hormone-Related Therapy
Raloxifene (Evista®) is a selective estrogen receptor modulator that joins estrogen and testosterone in this category. Even though estrogen therapy has been linked to an increased risk of blood clots, some malignancies, and heart disease, it is still commonly used to alleviate the symptoms of menopause and in younger women. Testosterone may be recommended to improve bone density for men with low testosterone levels.
Raloxifene has a similar effect on bones as estrogen. The medicine is administered once a day and comes in tablet form. To certain women, the use of raloxifene to treat osteoporosis may also be a means of lowering their chance of developing breast cancer. In cases of osteoporosis, raloxifene treatment often lasts for five years.
Salmon calcitonin (Fortical®, Miacalcin®) is a man-made hormone. The risk of spinal fractures is decreased, but not necessarily that of hip fractures or any other kind of break. Intramuscular injection or nasal inhalation is also a possible administration route.
The inhaled formulation might cause side effects such as a stuffy nose, nosebleeds, and headaches. The injectable type has more serious side effects, including rashes and flushes. It would be best if you did not consider this option initially. However, there is a rare but real chance of more severe side effects, such as a probable association with cancer.
-
Bisphosphonates
Bisphosphonates, a class of medications used to treat osteoporosis, are antiresorptive. These substances halt bone resorption. After three to five years, you might be able to quit taking bisphosphonates and still reap the benefits. These medicines are also accessible in generic form. Only females should use Boniva and Atelvia; males can safely utilise the rest of these items.
-
Biologics
Injectable denosumab (Prolia®) is available for both sexes and is administered every six months. When other treatment options have been exhausted, this one is often used. For some patients with impaired kidney function, denosumab is still an option. The possibility of severe adverse effects means that the long-term implications are still unknown. These might range from dangerous infections to issues with the thigh or jaw bones.
-
Anabolic Agents
Products like this help those who have osteoporosis regain bone mass. To date, three of these products have been granted market approval:
- Postmenopausal women at high risk of fracture can now take romosozumab-aqua (Evenity®). The product promotes bone growth and inhibits bone resorption. Once a month, you will receive two injections that will be given immediately, one after the other. Injections like these can only be provided once a year.
- The injectable medications teriparatide and abaloparatide are used once daily for two years. In many respects, these parathyroid products can be compared to actual hormones.
Can Osteoporosis Be Cured
Can osteoporosis be cured? While osteoporosis cannot be cured, it can be managed with various dietary, exercise, and other lifestyle changes that reduce bone loss. Medications to stimulate bone formation and inhibit further bone loss may also be recommended by your doctor.
Medications like estrogen replacement therapy are sometimes administered to female patients. Bone formation and bone density regulation are two of estrogen’s many functions in the body. Since estrogen levels in women naturally decline throughout menopause, this may explain why postmenopausal women are at increased risk for this disorder. Additional unpleasant menopause symptoms, such as hot flashes, may be alleviated by estrogen hormone therapy.
How to Prevent Osteoporosis
How to prevent osteoporosis? You can help prevent osteoporosis by changing some risk factors, including your food and lifestyle. Hormone therapy, which includes the replacement of lost estrogen, is also an effective defence against osteoporosis in postmenopausal women.
-
Diet
It would help if you had a calcium-rich diet all through life to keep your bones strong and healthy. There are 300 milligrams of calcium in a cup of low-fat or fat-free milk. Supplement users should know that their bodies can simultaneously absorb only 500 milligrams of calcium.

Vitamins & Minerals for Strengthening Bone
Because it makes calcium more easily absorbed by the body, vitamin D is an essential nutrient. Please see below the vitamin D RDIs established by the Institute of Medicine. One source of vitamin D is milk fortified with the vitamin, but getting some sunlight contact a few times each week is also good.
Discuss these figures with your healthcare physician. You may hear the advice to up your vitamin D intake. Your healthcare professional may also have recommendations regarding the form of calcium to take. For instance, you may be instructed to take calcium citrate rather than calcium carbonate. Calcium citrate is an alternative to antacids since it can be effective without stomach acid.
-
Lifestyle
Bone loss can be mitigated by sticking to a healthy routine. Get on a regular exercise schedule. Walking, running, and weightlifting are excellent ways to strengthen your bones since they all require the muscles to fight against the pull of gravity. Do not indulge in alcoholic beverages. Avoid it totally.Caffeine is safe, but too much of it can be dangerous. Avoid using cigarettes in any form.
How Does Physical Therapy Help Osteoporosis?
Seeing a physical therapist following an osteoporotic fracture may be beneficial. While physical therapy won’t fix the fractured bone, it will improve your chances of healing quickly and completely. A bone fracture is not necessary to begin a physical therapy regimen. You can take preventative measures against osteoporosis by attending physical therapy if you have been warned that you are at a high risk of developing the condition.
Your therapist will design your osteoporosis-specific physical therapy regimen. Your doctor will customise your rehabilitation plan based on age, current physical fitness level, and individual risk for fractures. Weight-bearing exercises and resistance training are common components of physical therapy for bone strength (such as weightlifting or yoga).
Your physiotherapist will work with you to enhance your balance and posture to reduce the risk of future fractures. Gaining mastery of your balance will aid in avoiding accidents. Plus, avoiding unnecessary bending and twisting of the spine is another benefit of practising good posture that can help prevent the occurrence of a spinal fracture.
Your physical therapist may suggest alterations to your dwelling and place of employment to aid healing. Your doctor will also instruct you to lie and sneeze safely to protect your bones.
Osteoporosis can be treated well without surgery using physical therapy, which may improve mobility, function, and bone strength. A physical therapist can help you reduce your risk of an osteoporotic fracture by teaching you bone-strengthening exercises and methods to modify your everyday routine.
Conclusion
Osteoporosis weakens bone that causes bone loss faster. Here in this article we have provided complete information about who is at risk for osteoporosis more. Luckily you can prevent this condition by taking precautions and keeping your body healthy.
How can you book an appointment?
We aim to see you within 24 hours so contact us to make an appointment either online at www.primphysiocare.co.uk or to find out more information on how we can help you, please call us on 07515280990 or email us primephysiocareluton@gmail.com. We are one of the best clinics whose physios are registered with HCPC, CSP and Physio first as well have enormous experience.
Frequently Asked Questions
Q. Who is at the highest risk for developing osteoporosis?
A. Osteoporosis strikes people of all ethnicities and sexes. Women of color, particularly those white or Asian and past menopause, are at an increased risk.
Q. To what extent do the following three things contribute to osteoporosis?
A. If you are a woman, you have a higher risk of osteoporosis. Because of hormonal shifts during menopause, women often have weaker bones and experience accelerated bone loss compared to males.
- Age. The probability of developing osteoporosis increases with age. As you age, your bone density drops, and your strength decreases.
- Definition of body mass. Women with weak skeletons and smaller frames are at a higher risk.
Q. What is the main sign of osteoporosis?
A. If osteoporosis has damaged your bones, you may have symptoms such as back pain due to a broken or collapsed vertebra—a gradual ageing-related diminution in stature. You are having a hunched back.
Q. Which foods are known as bone-breakers?
A. Consuming foods high in sodium (salt) leads your body to excrete calcium, which can accelerate bone loss.
Q. Doing what wrong things can worsen osteoporosis?
A. Don’t try these workouts if you have osteoporosis: Heavy lifting. Fractures can occur in bones that are already weak from activities like jumping, running, or jogging. Don’t move in sudden, jarring motions.