Lifestyle Changes for Preventing Postmenopausal Osteoporosis
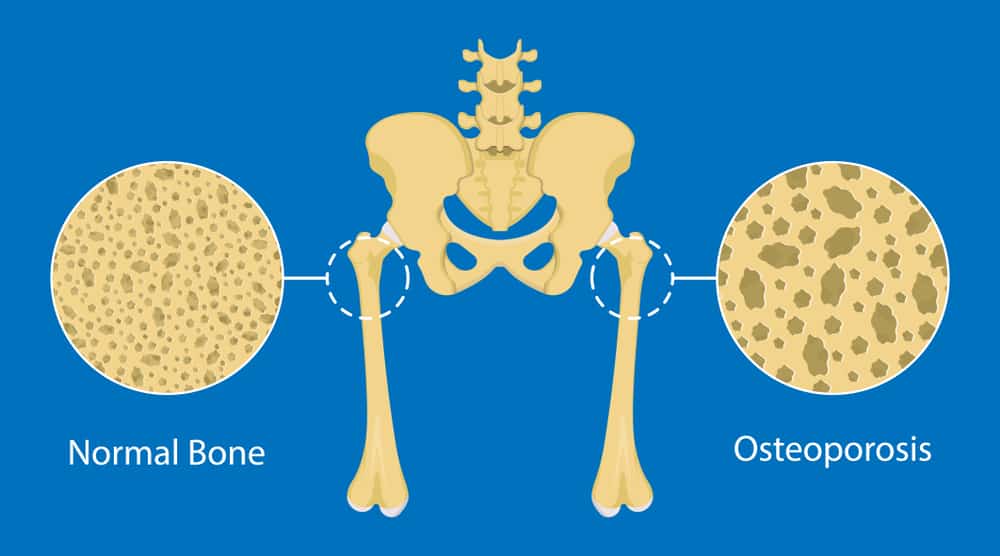
Postmenopausal Osteoporosis is a condition that can cause you Osteoporosis which is a bone disorder caused by weakened bone mass and density, increasing your risk of fractures.
Our lifestyle is a crucial element of how our health looks. Research shows that 80% of people who maintain a healthy lifestyle are less prone to illness or diseases. A healthy lifestyle brings you more health and prosperity.
Osteoporosis is the weakening of bones. Regrettably, there is no treatment available, But you can prevent this condition by your healthy lifestyle. Women are more affected by this condition because it is seen that pregnancy, lactation, and menopause cause a lot of calcium deficiency.
Women who do not take an adequate amount of calcium may suffer from these bone-weakening diseases that can cause further complications. Lifestyle Changes for Preventing Postmenopausal Osteoporosis are necessary as they can keep you safe from this bone-weakening disease.
What is Postmenopausal Osteoporosis, and who is at risk for Developing it?
Postmenopausal Osteoporosis is a condition that can occur in women after they have gone through menopause. It happens when the bones become thin and weak and can break easily.
Postmenopausal Osteoporosis is a heterogeneous disorder characterized by a progressive loss of bone tissue. This loss of bone tissue begins after natural or surgical menopause and leads to fracture within 15–20 years of the cessation of ovarian function.
Although age-related bone loss and suboptimal skeletal development (also known as “low peak bone mass”) may be contributing factors. It is believed that the leading cause of this condition is an increase in bone resorption that occurs in the first 5 or 10 years after menopause.
The primary pathogenetic factor of this condition seems to be hormone-dependent bone resorption and accelerated bone mass loss in the first five to ten years after menopause.
Postmenopausal Osteoporosis can be prevented by maintaining a healthy weight and exercising regularly. This is because of the increase in degranulation that occurs in the first 5 or 10 years after menopause and the rapid loss of bone mass that occurs in the first 5 or 10 years after menopause.
Osteoporosis occurs more in women than in men. Bone mineral loss rates increase after menopause. It happens with circulating estrogen associated with bone loss rates; the existence of a relationship between circulating estrogen and rates of bone loss, as well as the bone-protective effect of estrogen replacement concerning both bone loss and fracture in women. These are all vital pieces of evidence that suggest estrogen deficiency plays a significant role in postmenopausal bone loss.
The degree of bone metabolism, the rate and extent of bone loss, linked disease processes that generate a bone loss, and the amount of bone replaced each year are all essential factors. Age, menopause and the bone mass acquired at skeletal maturity all play a role in determining the prospective fracture risk for any postmenopausal female.
While there is no cure for postmenopausal Osteoporosis, you can take several steps to prevent the condition. Here we’ll discuss all aspects of lifestyle Changes for Preventing Postmenopausal Osteoporosis and how to clear your risk of developing this condition.
Symptoms of postmenopausal Osteoporosis
In the early phases of bone loss, a person usually will not have any symptoms. However, if Osteoporosis has compromised your bones, you may begin to experience signs and symptoms such as the following:
- Discomfort in the back as a result of a broken or collapsed spine
- Height reduction as a result of aging
- A hunched-over stance
- A bone that fractures significantly more quickly than one would anticipate.
How to prevent Osteoporosis after menopause
Adhering to these practices after menopause will reduce your risk of developing Osteoporosis, which is excellent news.
-
Osteoporosis prevention Diet
One is to make sure that you get enough calcium in your diet. You can get calcium from milk, cheese, yogurt, and dark leafy greens such as kale and spinach. Other good sources of calcium include salmon, sardines, and bone-in chicken.
Another way to prevent Osteoporosis is to get enough vitamin D. Vitamin D helps the body absorb calcium. You can obtain vitamin D in food such as fish like tuna, salmon, mackerel, fortified milk, and cereals. You can also get vitamin D from exposure to sunlight.
-
Osteoporosis prevention exercises
Exercise is also essential for preventing Osteoporosis. Weight-bearing exercises such as walking, running, and helping strengthen bones and slow the rate of bone loss.
Talk to your physician about other things you can do to prevent Osteoporosis. They may recommend medications such as bisphosphonates or denosumab, which can help slow the rate of bone loss.
First-line treatment for postmenopausal Osteoporosis
First-line treatment for postmenopausal Osteoporosis typically includes lifestyle changes and medications. Lifestyle Changes Preventing Postmenopausal Osteoporosis, such as getting enough calcium and vitamin D, exercising, and quitting smoking, can help prevent further bone loss. Medications such as bisphosphonates and denosumab can also help slow the rate of bone loss.
Other treatment options for postmenopausal Osteoporosis include hormone therapy and bone densitometry. H hormone therapy can help reduce the risk of fractures in postmenopausal women. Bone densitometry is a test that measures the density of your bones and can help identify areas of bone loss.
Hormone therapy:
Hormone therapy is a treatment option for postmenopausal Osteoporosis. H hormone therapy can help reduce the risk of fractures in postmenopausal women. There are two types of hormone therapy:
Estrogen therapy and bisphosphonate therapy
Estrogen therapy:
Estrogen therapy is a treatment option for postmenopausal Osteoporosis. E estrogen therapy can help reduce the risk of fractures in postmenopausal women. There are two types of estrogen therapy: oral estrogen therapy and topical estrogen therapy.
Oral estrogen therapy:
Oral estrogen therapy is a treatment option for postmenopausal Osteoporosis. O al estrogen therapy can help reduce the risk of fractures in postmenopausal women.
Topical estrogen therapy:
Topical estrogen therapy is a treatment option for postmenopausal Osteoporosis. Topical estrogen therapy can help reduce the risk of fractures in postmenopausal women.
Bisphosphonate therapy:
Bisphosphonate therapy is a treatment option for postmenopausal Osteoporosis. B bisphosphonate therapy can help reduce the risk of fractures in postmenopausal women.
Bone densitometry:
Bone densitometry is a test that measures the density of your bones and can help identify areas of bone loss. Bone densitometry is a safe and painless test that uses x-rays to measure bone density. A bone densitometry test can be done at your doctor’s office or a hospital.
If you have Osteoporosis, talk to your physician about the best treatment options for you.
5 ways to prevent Osteoporosis
Here we have discussed 5 ways to prevent Osteoporosis.
- Get enough calcium and vitamin D:
Calcium is essential for bone health. You can get calcium from milk, yogurt, and dark leafy greens such as kale and spinach. Other good sources of calcium include broccoli, collard greens, and turnip greens.
Vitamin D helps your body absorb calcium. You can get vitamin D from foods, including fish such as tuna, salmon, mackerel, fortified milk, and cereals. You can also obtain vitamin D directly from the sun.
- Exercise regularly:
Exercise is essential for bone health. Weight-bearing exercises such as stair climbing, running, and walking help strengthen bones and slow the rate of bone loss.
- Quit smoking
Smoking increases the risk of Osteoporosis, so quitting will help reduce your risk. Quitting smoking can be great for your bones since it helps prevent bone loss caused by smoking, which is one of the worst things for your bones.
Smoking increases the risk of Osteoporosis, so quitting will help reduce your risk.
- Avoid alcohol intake
Drinking alcohol can increase the risk of Osteoporosis thus avoiding it..
- Have a Regular Checkup
Having a regular checkup with your physician will help you prevent many diseases. Apart from having a healthy lifestyle, you should have a regular blood test so you may prevent osteoporosis.
How To Prevent Osteoporosis Naturally?
One risk factor for Osteoporosis that you cannot change is your age. Some risk factors, such as an inherited predisposition to Osteoporosis or a history of bone fractures, a tiny frame (the bones of persons with short frames tend to be lighter and thinner), or menopause, are mainly out of your control. On the other hand, you can delay or prevent Osteoporosis by adjusting a few risk factors. These are:
Diet
Our bones require specific nutrients for proper development, continued good health, and vitality into old age. These vitamins and minerals include calcium in varying amounts. Nevertheless, phosphorus, potassium, zinc, manganese, protein, and vitamins D, K, C, and A are all beneficial to the health of your bones.
Green vegetables:
Green vegetables are a rich source of essential vitamins and minerals, They should be added to your diet.
The magnesium and potassium in sweet potatoes neutralize the acids in your body, which can take calcium from your bones.
Nuts: They have reasonable amounts of calcium, potassium, and magnesium, whether fresh or dried.
Citrus fruits: You can include oranges and lemon in your diet, These citrus fruits can provide the entire daily requirement of vitamin C.
Fatty Fish: Salmon and other fatty fish are all excellent sources of vitamin D and omega-3 fatty acids. There is a lot of calcium and potassium in almond butter.
Almond, coconut, and oat milk have added vitamins and minerals.
Dairy Products: Milk and other dairy goods Dairy products, such as yogurt, cheese, and milk, are rich sources of calcium and contribute significantly to developing healthy bones.
Exercise:
Two exercises are best for building and keeping bone density, which can help prevent Osteoporosis.
- Exercises in which you use more of your body weight. Activities like jogging, aerobics, tennis, and dancing are some examples.
- Exercises that build strength or resistance include pushups, squats, and lifting weights.
Bones get stronger because these exercises naturally put them under stress.
Regularly doing any of these exercises can also help improve balance and coordination, which can help prevent falls that can break bones. YO ga, standing on one leg, and Tai Chi are good ways to improve balance.
Lifestyle Choices
Avoid alcohol and cigarettes to help prevent Osteoporosis. Studies show that drinking alcohol over a period, especially if it starts in adolescence or early adulthood, is terrible for bone health and raises the risk of Osteoporosis. Smokers are also more likely to get Osteoporosis because nicotine can change how calcium from calcium-rich foods is absorbed and used to strengthen bones.
Bone Loss After Menopause
In both the pre-menopausal and postmenopausal stages of life, a woman’s primary concern should be centered on preserving her bone mass as much as possible. Menopause is associated with a considerable acceleration of bone loss and an increased risk of Osteoporosis. According to research, up to 20% of bone loss can occur throughout these stages, and Osteoporosis plagues nearly all women over the age of 60 around the world.
Most postmenopausal women will break a bone at some point in their lives, and one in two will develop Osteoporosis bone loss after menopause. Fractures, often fractured bones, are painful injuries that restrict mobility and impair function. Fractures are linked to a decline in one’s quality of life and an increased risk of death.
Osteoporosis treatment can be started anytime; older women are more likely to respond positively to treatment if it is started earlier in the disease’s progression. Your treatment plan’s primary objectives are to reduce the risk of bone loss after menopause and to ensure that your bones continue to be healthy.
How does Osteoporosis impact Daily life, and what can be done to make living with the condition Easier?
When you discover that you have Osteoporosis for the first time, you could experience some anxiety. This would be the case if the diagnosis was determined to result from something known as a low trauma fracture. This indicates that you shattered a bone following an incident that did not appear severe or may have followed no incident.
If something like this happens, you most likely take additional precautions to prevent breaking any more bones. Because you were concerned about breaking a bone, you could believe you have no choice but to give up on things important to maintaining a high quality of life for yourself.
You can give up your regular workout program or steer clear of walking outside to reduce the risk of falling and breaking bones. You could even avoid visiting public places like shopping malls and movie theaters, where you have a greater chance of being shoved or bumped by other people.
If this is the case, you must make an effort to control your anxiety and not let Osteoporosis prevent you from participating in the things that you usually enjoy. Please make an effort to discover different approaches in which you can maintain the activities in which you take pleasure. It is necessary to keep up a high standard of living.
Conclusion
One in three women who have gone through menopause has Osteoporosis. Their lifetime risk of fragility fractures is higher than their lifetime risk of breast cancer.
Changes to a healthy lifestyle can lower the risk of osteoporosis and fragility fractures. These include getting enough calcium, vitamin D, and protein in your diet, getting regular weight-bearing exercise, giving up alcohol and smoking.
Guidelines for the diagnosis and treatment of Osteoporosis in postmenopausal women say that all women over 50 should get at least 1000 mg of calcium and 800 IU of vitamin D.
This can lower the risk of Osteoporosis is essential to create programs encouraging lifestyle changes and exceptionally balanced nutrient intakes.
How can you book an appointment?
We aim to see you within 24 hours so contact us to make an appointment either online at www.primphysiocare.co.uk or to find out more information on how we can help you, please call us on 07515280990 or email us primephysiocareluton@gmail.com. We are one of the best clinics whose physios are registered with HCPC, CSP and Physio first as well have enormous experience.
Frequently Asked Questions
Q. Which change to your lifestyle can help lower your risk of Osteoporosis?
Ans. Lifestyle changes like eating right, getting enough vitamin D, and exercising can help prevent Osteoporosis.
Q. Can Osteoporosis be fixed after menopause?
Ans. No, Osteoporosis can’t be reversed entirely and isn’t considered curable. However, there are several changes you can make to your health and lifestyle that can help slow bone loss. Your doctor can also prescribe you medicine to help rebuild your bones and slow down the loss of bone mass.
Q. What kinds of foods weaken bones?
Ans. Excess salt.
Hydrogenated oil.
Alcohol.
Vitamin A-rich foods.
Soft drinks.
Q. Can I make my bones stronger?
Ans. You can’t regain your bone density when you are young, but you can stop your bones from getting thinner quickly, even after you’ve been told you have it.
Q. What is the best osteoporosis prevention diet?
Ans. The best diet for the prevention of Osteoporosis includes food rich in calcium and vitamin D.
Q. Which are the two best osteoporosis prevention exercises?
Ans. The two best osteoporosis prevention exercises are
Physiotherapy: It strengthens your bones and increases flexibility.
Weight-bearing exercise: It also strengthens your bones.