Challenges in Diagnosing the Cause of Sciatica
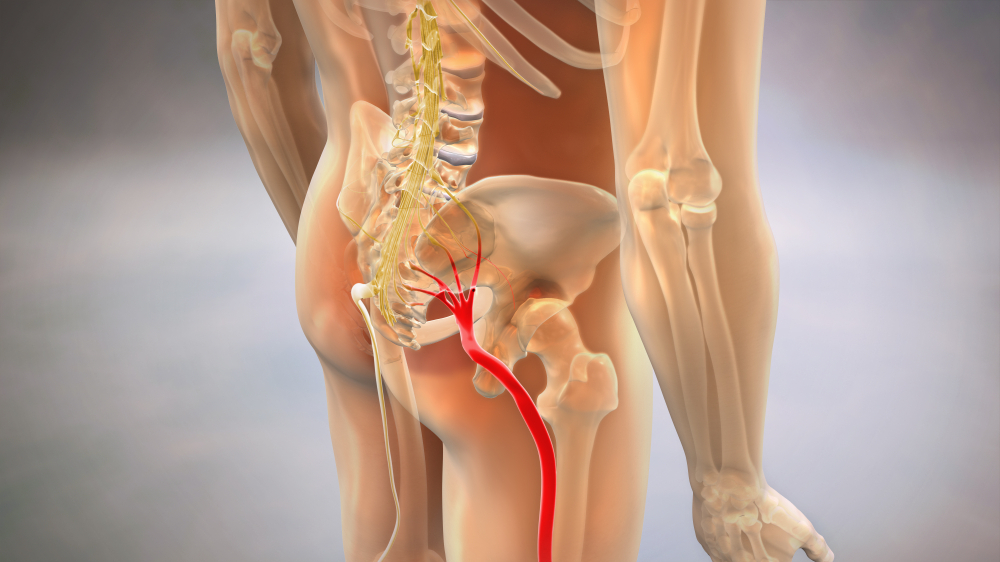
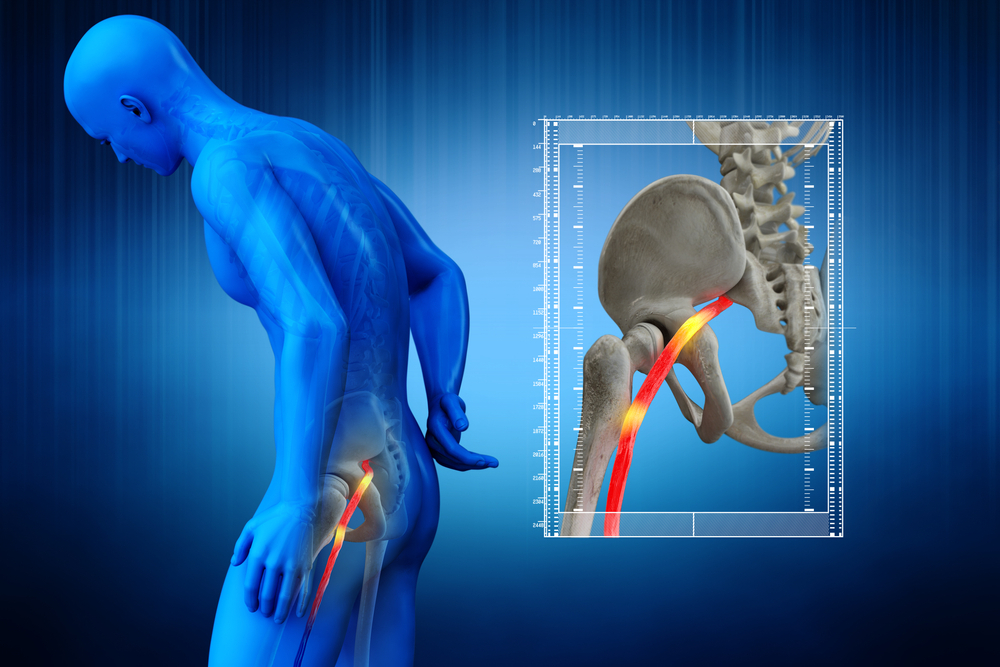
Diagnosing the cause of sciatica is vital and it’s necessary for the early treatment and recovery from it. Sciatica is a painful condition that could develop along the sciatic nerve path. The sciatic nerve branches off and runs down both legs from the buttocks and hips. When a herniated disc or bone spur presses on a nerve, the result is typically sciatica. As a result, the affected leg experiences swelling, discomfort, and even numbness. Even though sciatica pain can be excruciating, most instances resolve within a few weeks of treatment. Individuals with severe sciatica who also experience significant limb weakness or bowel/bladder abnormalities may require surgical intervention.
To effectively treat sciatica and alleviate pain, it is crucial to determine its aetiology. Medical history and a physical exam are standard procedures when diagnosing sciatica. Diagnostic nerve blocks and other medical imaging tests may be necessary for specific situations.
Every possible source of sciatic pain comes with its diagnostic difficulties and misdiagnosis risks. Herniated discs and degenerative spinal stenosis in the lumbar region are the common diagnosing cause of sciatica. The challenges in diagnosing these conditions are:
Sometimes the results of medical imaging tests don’t correlate with the symptoms that patients report. It’s possible that the patient’s symptoms and signs won’t line up with the results of the medical imaging.
A herniated disc can irritate the nerve root in the area if, for instance, tiny tears in the disc’s outer layers, the annulus fibrosus, allow inflammatory chemicals to flow out. Sciatica could result from this inflammation, although a diagnostic finding could not back up the symptoms. Two conditions may be present at the same time. Sheared discs in the lumbar spine can cause sciatica, which can mimic the symptoms of degenerative spinal stenosis in the same area. Images may demonstrate both diseases, but only one may be responsible for the signs. Because the treatment choices for sciatica depend on the underlying cause, a correct diagnosis is crucial for long-term pain alleviation.
Last Stages of Sciatica
Acute sciatica typically does not require medical attention if the symptoms are minor and do not last more than 4-8 weeks. A doctor could speed up the diagnostic process with the patient’s full medical history. Basic sciatic nerve stretching exercises will also be recommended by doctors. Pain that shoots down the leg during the workout is a common sign of the last stages of sciatica.
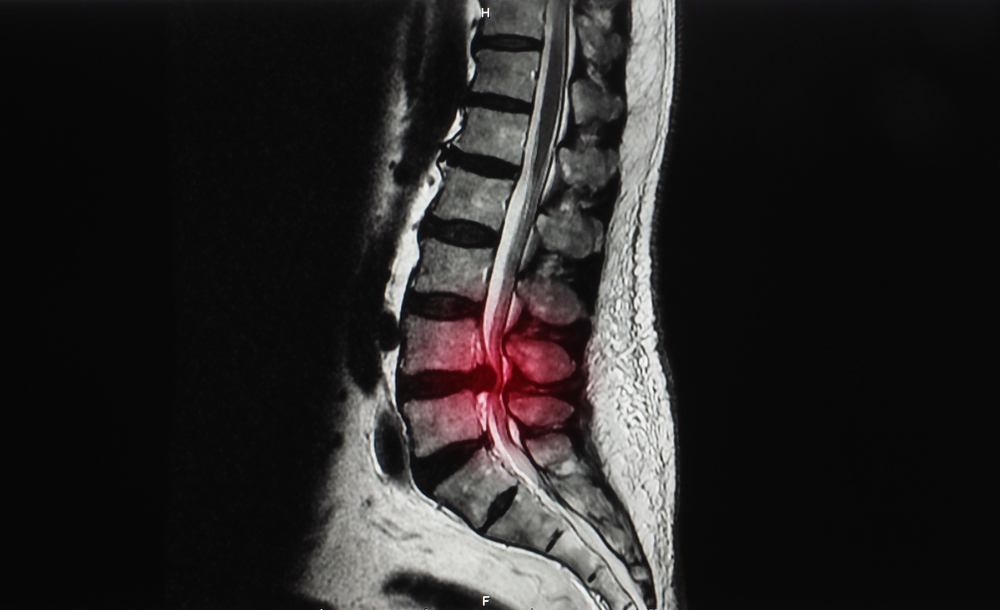
Imaging examinations like an X-ray or MRI may be required to determine what is pinching the sciatic nerve and causing the symptoms if the pain lasts longer than 4-8 weeks. Damage to the sciatic nerve can cause tingling, numbness, and, in extreme cases, weakness in the legs and knees. If left untreated, numbness and weakness will worsen and possibly become permanent.
Moreover, getting medical help immediately is essential if you’re experiencing nerve compression. If you’ve seen a gradual decrease in leg strength or numbness, the nerve in your leg may have been injured. Surgery may be necessary if the pain and other symptoms of advanced sciatica (when the nerve is crushed) are severe.
Physical Therapy to Treat Sciatica
As part of a comprehensive approach to treating your sciatica, your spine specialist may recommend visiting a physical therapist. Both passive and active therapies are frequently used in physical therapy. Physical therapy can be either “passive” (the patient receives treatment from the therapist, such as with heat or cold packs) or “active,” in which the patient actively engages in the treatment process (e.g., therapeutic exercise).
Reduces inflammation and pain, boosts physical performance, and stops sciatica from returning. In addition, you may learn how to improve your posture as part of your physical therapy. Many people also take home exercise programs to continue their progress toward better health.
Impact Of Physical Therapy
The physical therapist will ask questions about your sciatica and medical background at your initial appointment. Your doctor may question your activity level before low back and leg discomfort onset and the date you first experienced sciatica.
Your physical therapist will likely have you complete several rudimentary exercises to gauge your mobility, posture, reflexes, and other attributes. You could be required to twist at the waist, bend at the knees, flex at the waist, or bend from side to side. You are walking while being observed by the therapist. Your therapist will be able to evaluate your current state and the extent to which sciatica limits your physical functioning during this examination phase.
The information your PT gathers during the evaluation is then used to create a well-thought-out plan for your PT sessions. The objectives of your passive and active therapy plan are attainable and reasonable. Your treatment plan may include new stretches and exercises as your back, and leg pain decreases and becomes more bearable.
Like many other treatments, physical therapy is not a quick fix and may take weeks or even months to see positive benefits. Your physical therapy treatment plan will likely incorporate in-clinic sessions with your PT and an at-home exercise program.
Sciatica Reduced by Passive Physical Therapy
To prepare your body for active therapies that increase strength, flexibility, and long-term pain avoidance, passive physical therapy aims to gently remove unpleasant soft tissue tension by relaxing your body. Some or all of the following treatments may be a part of your specific passive PT regimen.
-
Deep Tissue Massage
Deep tissue massage relieves tension in the muscles and fascia (muscular connective tissue) that can pressure the sciatic nerve and its branches when applied to the low back, hips, and buttocks. The therapist will use direct pressure and friction (ligaments, tendons, muscles) to alleviate the strain on your strengths and other soft tissues.
-
Hot And Cold Therapies
The goal of using heat during physical therapy is to increase blood flow to the affected location, increasing oxygen and nutrition delivery to the tissue. For instance, a heat pack applied to the piriformis muscle may alleviate the muscle spasms that are likely the root of your sciatica. The opposite is true with cold therapy, which helps reduce inflammation, muscle spasms, and discomfort by slowing circulation. The best results from heat and cold treatments are achieved by alternating them. Therefore your physical therapist will do just that.
-
TENS
TENS is made possible by a machine that delivers electrical current to your muscles at varying (and safe) intensities. In addition to alleviating muscle spasms, transcutaneous electrical nerve stimulation (TENS) has been shown to stimulate the release of endorphins, the body’s painkilling chemicals. You certainly can if your therapist feels you’d benefit from using this at home. Your PT’s TENS unit will be far larger than your home unit. TENS units, however, can be beneficial regardless of size.
-
Ultrasound
Ultrasound uses sound waves to penetrate deep into muscle tissue, where they produce a soothing heat that promotes recovery by increasing blood flow. The symptoms of poor circulation, including muscle spasms, cramping, edema, stiffness, and discomfort, are alleviated by a boost in blood flow.
Causes of Sciatica
Painful symptoms such as tingling, numbness, and a burning sensation can develop when the sciatic nerve is compressed. The common diagnosing cause of sciatica includes spinal disc herniation and the development of bone spurs on the vertebrae. A tumour’s growth can occasionally squish a nerve. Diseases like diabetes can also damage the nerve. Additional reasons for sciatic pain can be:
- A condition characterised by narrowing the spinal canal in the lower back; also known as lumbar spinal stenosis.
- Spinal spondylolisthesis occurs when a disc protrudes forward and slides over the vertebra below it.
- Spinal tumors could put a strain on the sciatic nerve at its origin.
- A spinal infection that spreads through the body.
- There may be supplementary reasons, such as spinal cord damage.
- Rare yet life-threatening, cauda equina syndrome damages the nerves at the base of the spine.
- Often, one cannot pinpoint the root causes of sciatica.
Straight Leg Test for Sciatica
One frequent diagnostic tool for disc disease and nerve root irritation is the straight leg test for sciatica. Disc herniation and neural compression can both be detected with its help. Since it can identify abnormal stress on or reduce a nerve root, it also fits the bill for a neurodynamic evaluation. The name “Laseague’s test” comes from the fact that it was first described by League more than a century ago.
This examination causes traction on the lumbosacral nerve roots, especially from L4 to S2, and tensile strains on the sciatic nerve. During SLR, the dura mater is dragged caudally, laterally, and anteriorly, which exerts an anterior and inferior force on the nerve roots. The sciatic foramen, the sacrum, the nerves that cross the pedicles, and the intervertebral foramen are all sequentially pulled under tension from the sciatic nerve. Localised pain or soreness near the larger sciatic notch is a common symptom.
How to Diagnose Sciatica at Home
How to diagnose sciatica at home? Sciatica can be evaluated on your own time. Most people have heard of sciatica, a pain in the lower back that travels down the leg and occasionally to the foot. At the same time, it may be difficult to believe most cases of sciatica resolve independently within three months of beginning conservative treatment, even in the most severe cases. It’s vital to get a clinical diagnosis from a doctor for diagnosing cause of sciatica if you’re experiencing pain in your buttocks or leg or if you’re experiencing numbness or other neurological issues in your leg.
-
Differential Diagnosis of Sciatica
A physician will likely evaluate your muscular strength and reflexes during the physical examination. Examples of differential diagnosis of sciatica include:
- Standing on one’s toes or heels.
- Getting up from a squat.
- Lifting one’s legs off the ground while lying on one’s back.
- Performing these moves almost always increases sciatic pain.
-
Tests
Individuals who are experiencing significant pain or whose pain has not diminished after a few weeks may require:
-
X-ray
In some cases, an X-ray of the spine will demonstrate that an excess of bone is putting pressure on a nerve.
-
MRI
This method can use a strong magnet and radio waves to create photographs of the back’s cross-section. Herniated discs and pinched nerves are visible on an MRI scan because of the MRI’s ability to create high-resolution images of bone and soft tissues.
-
CT Scan
Injecting a dye into the spinal canal before obtaining X-rays is a common part of CT scanning (CT myelogram). The spinal cord and nerves become more visible in imaging as the dye travels around them.
-
Electromyography (EMG)
The exam evaluates muscular activity and nerve signals. This analysis can determine the extent of a nerve root injury.
Sciatica Diagnosis and Treatment
What should you know about the sciatica diagnosis and treatment? Mild sciatica tends to heal on its own. If you are not feeling better after trying self-care, make an appointment with your primary care doctor. You should obtain help if the discomfort persists for more than a week, is severe, or worsens. Quickly consult a doctor for diagnosing cause of sciatica if you’re experiencing:
- Pain that comes on suddenly and stays in the lower back or one of the legs, along with tingling, weakness, or paralysis in the affected limb.
- Discomfort following a traumatic event, like a car crash
-
Physical Therapy
After discomfort has subsided, a doctor might devise measures to keep the patient from getting hurt again. Such programs’ posture, core, and range of motion exercises are common components.
-
Steroid Injections
Injecting a corticosteroid medicine near the painful nerve root can be effective in some circumstances. In many cases, a single injection is all that is needed to alleviate discomfort. Within a given calendar year, three awards may be bestowed.
-
Surgery
The surgeon can surgically remove the bone spur and the herniated disc tissue pressing on the nerve. However, surgery is often reserved for cases where sciatica has led to profound muscle weakness, bowel or bladder control loss, or persistent pain despite non-invasive therapies.
Latest Research on Sciatica
New treatment options may be available for those suffering from sciatica, which causes excruciating pain in the lower back and legs. This is an innovative spin on a standard treatment for hypertension: its use to alleviate sciatica. According to a randomized clinical trial and the latest research on sciatica conducted by researchers at the University of Utah Health, patients with sciatica who had physical therapy for four weeks had much less disability one year after their initial medical visit.
What Kind Of An Impact Does Sciatica Have On Your Quality Of Life?
Pain from sciatica can radiate from the lower back, down the back of the leg, and into the foot. The discomfort might be intermittent, lasting anywhere from a few hours to a few weeks. This could result in anything from a minor annoyance to severe pain that makes even going about daily life a struggle. If you suffer from sciatica, even sitting could be excruciating, besides being physically active and participating in sports.
When deciding whether or not to undergo surgery for sciatica, it’s essential to evaluate the level of discomfort experienced. It may be time to consider surgery if your continuous pain interferes with your career, hobbies, social life, or relationships.
Even though sciatica manifests initially as inflammation of the nerves, permanent nerve damage can occur. Damage to the sciatic nerve can cause tingling, numbness, and, in extreme cases, weakness in the legs and knees. If left untreated, numbness and weakness will worsen and possibly become permanent.
How can you book an appointment?
We aim to see you within 24 hours so contact us to make an appointment either online at www.primphysiocare.co.uk or to find out more information on how we can help you, please call us on 07515280990 or email us primephysiocareluton@gmail.com. We are one of the best clinics whose physios are registered with HCPC, CSP and Physio first as well have enormous experience.
Google FAQs
Where can I find information on diagnosing an issue with my sciatic nerve?
An accurate diagnosis of sciatica requires a patient’s medical history and a thorough physical examination. Patients typically report pain that spreads down their legs.
Asking a neurologist about sciatica: what can they do?
Pain medication and physical therapy are the first lines of defence for neurologists treating sciatica, followed by epidural steroid injections and referral for surgery. Anesthesiologists administer steroid injections or perform a selective nerve root block to treat sciatica.
Where does sciatica pain come from?
Pain in the sciatic nerve originates from a nerve in the lower back that has been irritated, inflamed, pinched, or compressed. The most typical culprit is a herniated or slipped disc that presses on a nerve root. Most cases of sciatica resolve spontaneously with rest and self-care.
If you have sciatica, who is the best doctor to see?
Extreme cases of sciatica are best treated by a neurologist or other physician with expertise in the nerve system. Your doctor may suggest seeing a specialist. Sciatica affects about 40% of the population at some point.
Where are injuries to the sciatic nerve most common?
Due to its more lateral position and relative tethering of the nerve course, the peroneal division of the sciatic nerve sustains more injuries than its tibial counterpart.