Sciatica
Sciatica is a term used to describe severe leg pain caused by a prolapsed lumbar disc pressing one of the lumbar spine’s nerve roots. Lumbar radiculopathy is the medical term for sciatica, which is also known as radicular pain or nerve root pain.
Sciatica is a condition where a person feels pain in one leg radiating from the lower back and hip joint generated by the compression of the sciatic nerve. Physiotherapy and exercise is the first hand treatment for sciatica to help soothe the patient of the pain. Sciatica has many patients thriving in pain in one of their legs and back.
People often misinterpret the common back pain and associate it with sciatica. They turn up to google and look for how it can be treated. Whereas, they also largely rely on google to diagnose their disease. Google provides them with a set of treatments which do them more harm than good and their pain continues to persist and become more painful over time. It is better to turn up to a physiotherapist or a general physician (GP) to better diagnose and treat your condition.
Different patients even show up at our clinic saying we have sciatica but how do they know on their own? It is better to always visit someone who has the proper knowledge of the disease. You can visit us regarding any problem you have. Our physio team will try its best to provide you with the apt exercises to treat your sciatica pain.
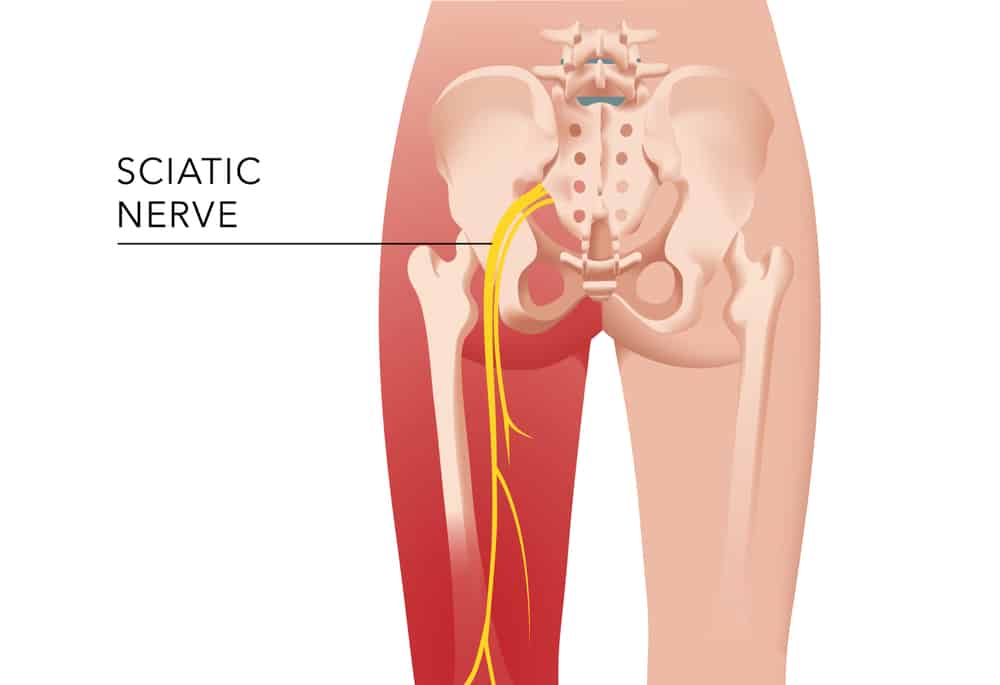
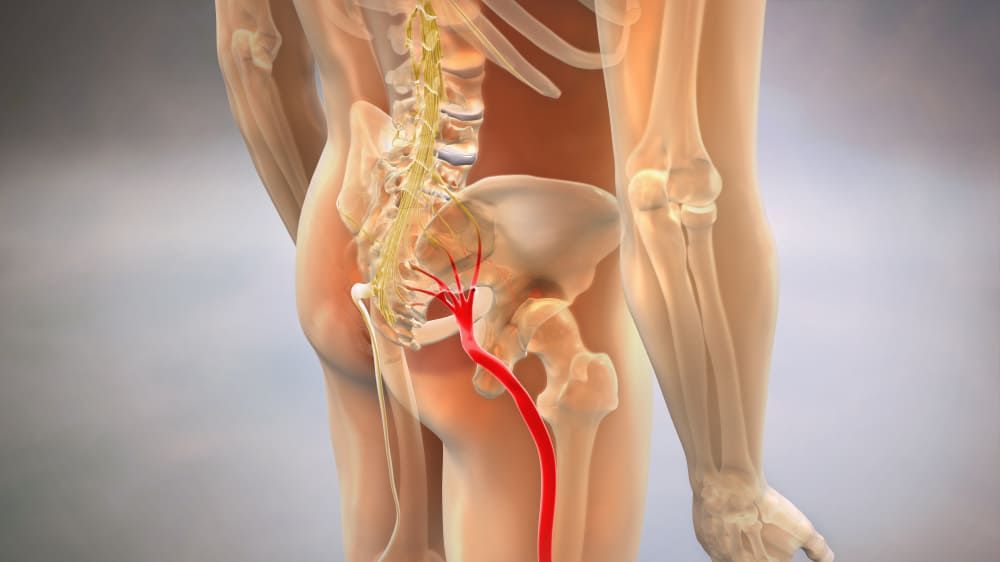
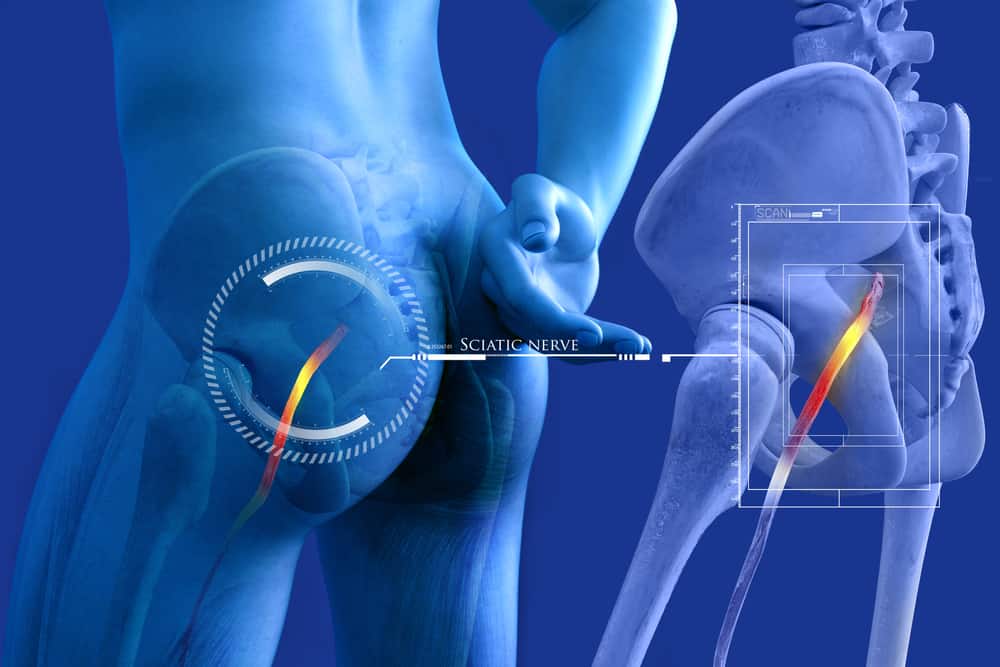
Sciatic Nerve
The sciatic nerve is the body’s biggest nerve. The sciatic nerve is made up of tiny nerve roots in the lower or lumbar spine that link together to produce a thick, rope-like nerve. It then runs down the back of the leg to the knee, passing through the buttock. It divides into smaller nerves that travel to various parts of the lower leg and foot.
A nerve’s chemicals and messages must be allowed to travel freely in both directions for it to function correctly. As we move, the nerve must be able to expand and slide across the tissues it travels through. The flow of these molecules is disrupted if it is pinched, inflamed, or jammed, and the nerve begins to produce symptoms.
Pain, tingling, numbness, coldness, or heat are all possible symptoms. Other strange sensations such as crawling ants or hot oil trickling down the leg may be experienced.
Confusion about sciatica
There is a lot of confusion regarding sciatica pain. Let us enlighten our readers with what actually sciatica is:
- Back pain isn’t very common to be found in many patient
- Sciatica is a type of leg pain that usually occurs below the knee. There must be soreness in the buttocks, thighs, calves, or feet. Burning, stinging, or surges of pain are all possibilities.
- Pain may be just in the leg or may be in all those above mentioned areas.
- It depends if back pain is there, if back pain is there it might be milder than leg pain.
- Most people do not need surgery.
- Most leg pain is not necessarily sciatic pain.
How Common Is Sciatica?
Sciatica is an extremely prevalent ailment. Sciatica affects about 40% of people in the United States at some point in their lives. Back pain is the third most prevalent reason for people to seek medical help.
It is not easy to get perfect figures as the data is collected in many different ways. According to studies, people who acquire sciatica at some point in their lives range from 12 percent to 43 percent. The percentage of people who experience sciatica (leg pain radiating below the knee) at any given time ranges from 2% to 13%. Sciatica affects about 5% to 10% of patients who suffer mechanical low back pain.
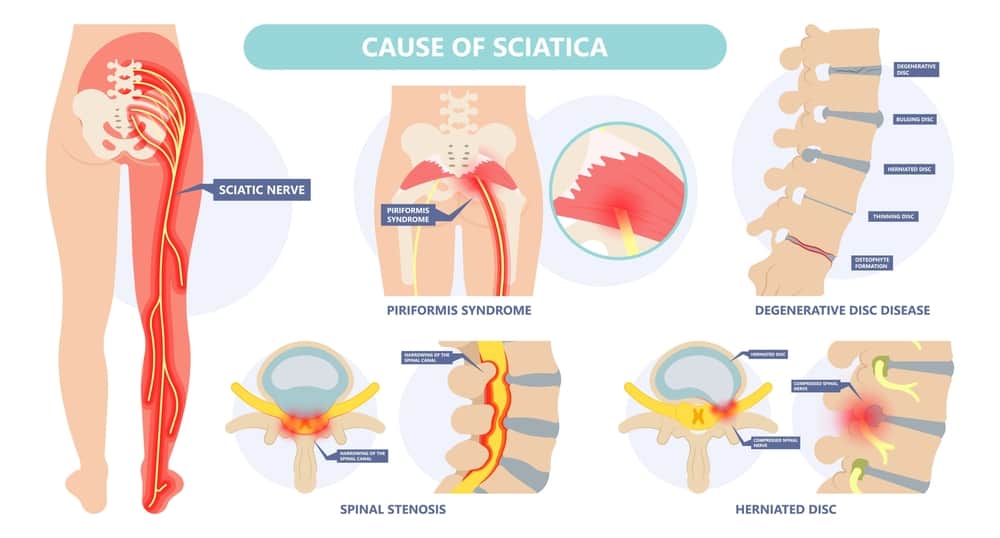
If you are wondering what causes sciatica? Let me give you a complete guide on causes of sciatica, so that you may prevent its forthcoming ‘as prevention is better than cure’. It can be caused by several different medical conditions :
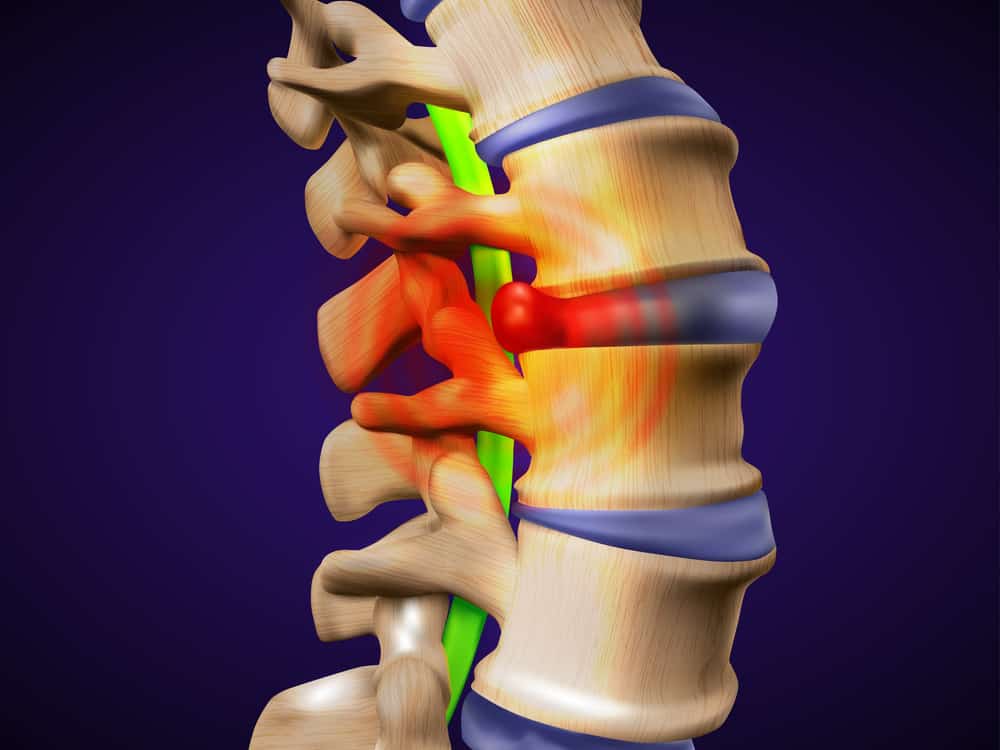
Pressure on a nerve root:
- This is the most common cause of sciatica.
- A herniated or a slipped disc pressurises the nerve root.
- Studies show about 1 to 5 percent of all people in the US have slipped discs at one point in their lives.
- The cushioning pads between each vertebra of the spine are known as discs.
- The gel-like centre of a disc can expand (herniate) through a weakness in its outer wall due to pressure from vertebrae.
- When a herniated disc happens in your lower back it presses against the sciatic nerve. This is direct compression.
- An acidic chemical irritant from the disc material (hyaluronan) may leak out and cause inflammation and irritation in the area around the sciatic nerve.
Spinal Stenosis :
- It is a condition in which abnormal narrowing of the spinal cord takes place.
- The space available for the spinal cord and nerves is reduced as a result of this narrowing. This pressurises the sciatic nerve.
Degenerative Disc:
- In this disease, the disc naturally wears down between the vertebrae of the spine.
- As the discs wear out, their height decreases, and the nerve passages become narrower (spinal stenosis).
- As the sciatic nerve roots leave the spine, spinal stenosis might squeeze them.
Spondylolisthesis :
- Spondylolisthesis is the misalignment of one vertebra with the one above it, narrowing the aperture through which the nerve leaves.
- The sciatic nerve can be pinched by the stretched spinal bone.
Osteoarthritis :
- In aged spines, bone spurs (jagged edges of bone) can occur and pressurise lower back nerves.
- Each vertebra is joined to the next one above and below by small joints either side called facets.
- Wear and tear, arthritis, and injuries can cause facets to become inflamed, causing them to enlarge and even produce extra spurs and bumps.
- This can irritate nerve roots by pressing on them.
Tumours:
- The sciatic nerve is compressed by tumours in the lumbar spinal canal.
Injury:
- Trauma injury to the lumbar spine or sciatic nerve.
- These injuries can cause sciatic pain.
Piriformis Muscles:
- Piriformis syndrome occurs when the piriformis muscle, a tiny muscle deep in the buttocks, tightens or spasms.
- This can irritate and press on the sciatic nerve.
- Piriformis syndrome is a rare neuromuscular condition.
Cauda equina syndrome:
- A bundle of nerves located at the end of the spinal cord called cauda equina are affected by this disease which is a very rare but serious condition.
- This syndrome produces leg pain, numbness around the anus, and bowel and bladder control problems.
Hamstrings:
- The hamstring muscle, like the piriformis, is intimately connected to the sciatic nerve and runs alongside it down the back of the leg.
- The sciatic nerve’s capacity to move and stretch may be affected by a hamstring injury or substantial tightness.
- It’s possible that, like the piriformis muscle, it’ll only aggravate an already sensitive nerve and cause discomfort in another region.
Who Gets Sciatica?
Most people who get sciatica are between the ages of 40 and 50. Women are more prone to it because of the pregnancy and the developing uterus which may compress the sciatic nerve.
With sciatica adults are at greater risk. Lifting weights and other strenuous activities, especially when twisting and bending, increase the risk of acquiring the illness. Another risk factor is whole-body vibration from machinery or automobiles.
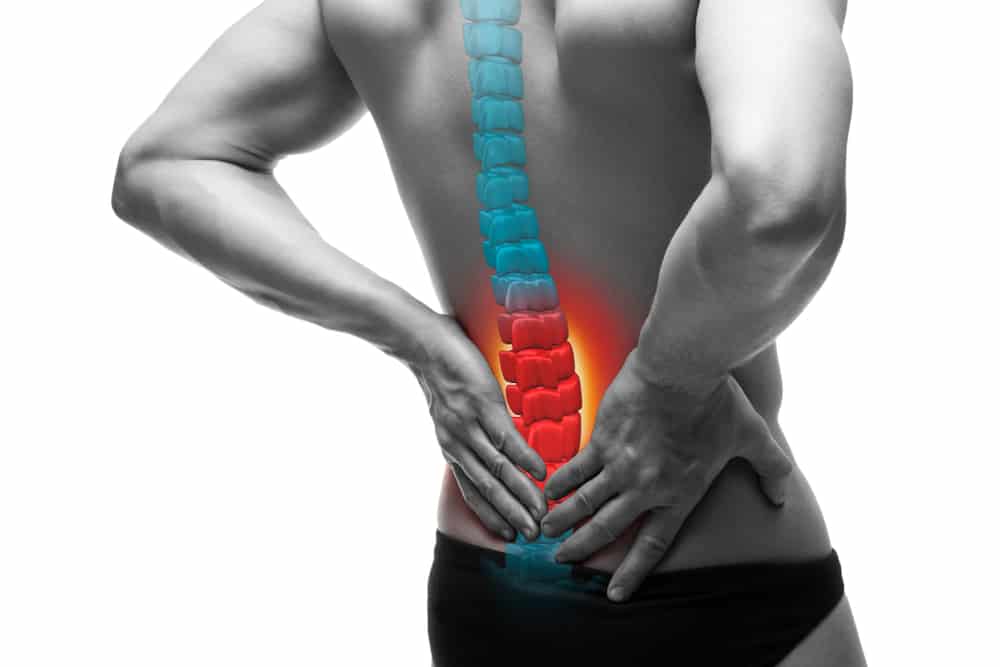
Sciatica Symptoms
The sciatica symptoms include:
- Pain in the lower back, buttocks, and down your leg that ranges from moderate to severe.
- Pain surges down the leg in waves.
- Lower back, buttocks, leg, or foot numbness or weakness
- There may also be muscle weakness and a lack of reflexes.
- Standing, sitting for an extended period of time, bending backwards, and coughing or sneezing exacerbate the symptoms.
- Pain that gets worse with movement; inability to move.
- Feeling of “pins and needles” in your legs, toes, or foot.
- Control of the bowels and bladder is lost (due to cauda equina).
Examination for Sciatica
When you go to the doctor with what you think is sciatica leg pain, he or she asks you a series of questions, performs tests, and thinks about whether you’re right or if you have something different because many people might associate leg pain with sciatica when actually it is not sciatic pain. They will ask a number of questions to find out what sciatica is according to you and what describes your sciatica symptoms best.
The symptoms of sciatica are usually really popular and well known and so your case should match that. If it doesn’t the doctor will look for alternative explanations.
- Sciatica is a painful condition that affects the leg.
- If there is back pain, it will not be the most prominent aspect.
- The pain will take several days or weeks to go away.
- The agony will be intense and unbearable, not just “a little leg ache.”
- The pain will be worse further down the leg than it would be higher up, and it will be worse by actions like sitting or bending.
- Activities that lower disc pressure, such as lying, will help to alleviate the pain.
If these questions are answered with a ‘Yes’, then these should confirm your sciatica pain. The examination should further approve it.
Examination
The doctors are looking for the affirmation of these symptoms with what they will examine. This will assure them that they are on the right track to the diagnosis. The examination should be based on following facts:
- The patient should be in pain and take steps to alleviate it as much as feasible. It’s not going to work if they’re scribbling on the floor or sitting slumped with a smile on their face.
- At least on the affected side, a straight leg raise (SLR), in which the doctor elevates the leg off the couch, should be positive. That is to say, the action should aggravate the patient’s sciatica pain.
- Any loss of sensation, muscle strength, or reflexes should be linked to the nerve that is thought to be causing the sciatica.
- The movement of the lumbar spine should be confined to a moderate or large extent.
If all of the results point to sciatica, or radicular nerve pain as it is officially known, the doctor may prescribe more tests. Magnetic resonance imaging, or MRI, is the most useful. MRI is especially useful for imaging soft tissues like discs and nerves, which are thought to be implicated in this case.
The location of pain, the SLR, and any loss of power, feeling, or reflexes should all be visible on an MRI scan, as should a disc bulge compressing the particular nerve. If this is the case, the doctor can be confident that they have made the accurate diagnosis and move on to treatment options.
Types and Diagnosis
Sciatica is mainly of 3 types depending on how long the symptoms take to fade away:
- Acute sciatica lasts typically less than 6 weeks.
- Subacute sciatica lasts between 6 to 12 weeks.
- Chronic sciatica is present for over 12 weeks and can be longer than that.
For mild episodes of pain diagnosis is not typically considered mandatory. However, people with intense and consistent pain will need a complete assessment from their doctor to rule out other causes of their sciatica pain and to help with pain relief.
Tests:
For further diagnosis they may also perform several tests. These include:
- They may perform spinal x-rays for spinal fractures, disk problems, infections, tumours and bone spurs.
- They may conduct nerve conduction velocity studies/electromyography to examine how well electrical impulses travel through the sciatic nerve and the response of muscles.
- To check the pain caused by vertebrae or discs they may conduct a myelogram test.
- To examine detailed images of the back’s bone and soft tissues, use magnetic resonance imaging (MRI) or computed tomography (CT) scans. An MRI can reveal nerve compression, disc herniation, and any arthritic condition pressing on a nerve. To confirm the diagnosis of sciatica, an MRI is frequently ordered.
The Prognosis For Sciatica – How Is It Going To Go?
Acute sciatic pain usually goes away on its own. The bulging disc which disturbs the alignment of vertebrae is reabsorbed. According to one study, half of acute sciatica patients improved in ten days and three-quarters in four weeks. It goes away with time and self care treatments.
Just to counter check, don’t forget to contact your health care provider or physiotherapist in case your symptoms are mellowed down or the recovery is not as smooth as expected.
Some people are not recovering as good as others, these include;
- Women who have weaker physical strength.
- People suffering from melancholy, stress, and anxiety, as well as dissatisfaction with their jobs, strenuous work, legal claims, and pessimism about returning to work.
- People with more severe pain and symptoms in the beginning of the disease.
How you can ease the pain yourself
More acute or milder sciatic usually gets better itself within a span of 6 weeks maximum. To help you with pain and speed up your recovery you can do these following things:
DO’S
- Maintain as much of your daily routine as feasible.
- Begin mild exercise as soon as you are able – anything that gets you moving will benefit you.
- Sciatica exercises should be done on a regular basis.
- Inquire with your pharmacist about pain relievers (paracetamol is unlikely to assist, and the effectiveness of NSAIDs in treating sciatica is unknown).
- When sleeping on your side, place a tiny, firm cushion between your knees; when sleeping on your back, place several firm cushions beneath your knees.
- Look after your posture, try to maintain it while sitting, and give your back proper support.
- Try getting a healthy diet.
- Apply heat packs to the hurting areas – these are available at pharmacies.
DONT’S
- Do not sit or lie down for a longer period of time, even if it hurts just get yourself moving as it may help you recover faster.
- Avoid using hot water bottles to ease the pain in case your skin is numb because you can scald yourself.
Sciatica Treatment
Sciatica treatment is possible if it does not go away on its own in 6 weeks time. Treatment options include:
- Localised heat or cold (with skin protection) may assist relieve spasms and pain.
- Pain relievers, beginning with paracetamol and advancing to heavier drugs when needed
- It is recommended that you return to work as soon as possible, rather than waiting until you are pain-free.
- Normal movement and activity may cause pain, but this is not hazardous. As the pain allows, activities should be progressively resumed.
- Bed rest should only be recommended if the pain is severe enough that it is necessary to lie down.
- After that, regular exercise and normal activities are required.
- Positioning may be more comfortable to lie on your back with your knees and lower thighs supported up by numerous firm pillows. If you’re lying on your side, a tiny pillow between your knees can help.
- Physiotherapists may suggest exercises and stretches to treat sciatica.
- Physiotherapy for sciatica is a must as it may include exercises and certain manual therapies to treat it.
- Your mental well being is also important and for this purpose they may provide you with psychological support.
Other Treatment Options:
If your pain is severe and your doctor’s therapies have failed, you may be referred to a hospital expert for:
- Painkilling injections (spinal corticosteroid to help ease pain).
- A technique to seal up some of your back’s nerves so they don’t convey pain signals
- Alternate therapies are a popular treatment as well which includes spine manipulation by a licensed chiropractor, yoga or acupuncture.
- Surgery might be handy- decompression surgery can occasionally help reduce sciatica.
If the pain does not settle then doctors may intervene with
If the pain is extremely sever and it doesn’t go away with anything then your doctor may intervene with following emergency options:
- They may calm the inflammation with a steroid injection called an epidural injection.
- In around 2 % of cases a discectomy operation may take place, in which the abnormal disc is removed.
- Nerve root blocks, similar to epidural but targeted at the nerve root where the problem lies.
What Are The Potential Complications Of Sciatica?
The potential risk factors or complications that often interfere with sciatica treatment are given below:
- Limited ability to do work which may ultimately lead to many offs from work or loss of job.
- Compression causes nerve injury. Due to a decrease of muscle power and sensation in specific places, a person may experience foot drop. This is the side effect of surgery. Which might interfere even with normal walking.
- Sciatica can also cause permanent loss of sensation in the affected leg due to nerve damage.
- Ongoing or long lasting pain is one of the complications of chronic sciatica.
- Life style is mostly affected.
- Psychological impact may also hinder a person’s mental health such as depression or anxiety.
How to stop sciatica coming back
You can prevent sciatica by following the instructions below:
DO’S
- Doing exercise regularly and staying active. It keeps your muscles flexible and joints in a working condition.
- Make sure you have a good posture when sitting and standing
- Use a safe technique when lifting heavy objects
- Sit correctly when using a computer
- Maintain a healthy weight. Lose weight if you’re overweight.
- Choose physical activities least likely to hurt your back: Consider low-impact activities such as swimming, walking, yoga or tai chi.
DONT’S
- Do not smoke because smoking can increase your risk of getting sciatica for it weakens the nerves and ligaments.
- Do not wear uncomfortable shoes which may cause you to fall.
Physiotherapy For Sciatica
The best non-invasive treatment for sciatica so far is physiotherapy and it is also recommended by the Department of Health’s National Institute of Health and Care Excellence (NICE), which is an expert on appropriate treatments. Still the physiotherapist should monitor the patient constantly and check the progress report.
The physiotherapist will develop a personalised treatment plan on the basis of general guidelines aimed at:
Relieving sciatica pain:
Sciatica pain can be alleviated in a variety of ways with the help of a physiotherapist. The tensions or irritation of the spinal nerve in question can be changed by mobilising or manipulating the spinal joints in the lower back. Sciatic pain can also be relieved by a deep massage of the piriformis muscle in the buttocks and piriformis stretches.
Spinal Flexibility Maintenance:
Muscle tightening and stiffness is another contributing feature. The ranges of motion in the lower back and adjacent areas are maintained through repeated movements and stretches. Stretching the lower back, piriformis, hamstrings, quadriceps, and other hip and pelvic muscles can be recommended by a physiotherapist.
Strengthening Exercises:
The whole stability and control of the chest is dependent on the lower back and pelvis. Thus improving its muscle strength might help support the trunk area better. It is beneficial to work on the core muscles, low back muscles, abdominals, and buttock muscles.
Aerobic Exercises:
Exercise has been demonstrated to be beneficial in the treatment of a wide range of pain disorders. The form of exercise you pick is unlikely to matter as long as you enjoy it and do it on a regular basis. Exercises such as fast walking, swimming, cycling, Tai Chi, Pilates, or gym work may be beneficial.
Improving Your Posture:
Poor posture not only affects one’s attitude, but it can also cause long-term stress to the lower back structures, aggravating pain.
Preventing Sciatica’s further Onset:
Even if no pain concerns exist, there are numerous reasons to establish excellent exercise, posture, and lifting habits. Although there is no evidence that following proper procedures will avoid sciatica episodes or their recurrence, it is worthwhile to do so.
Most Effective Exercises For Sciatic Pain
Having discussed the benefits of physiotherapy let us find out the most effective physio exercises for sciatic pain. You can also perform these at home for your sciatica pain. Following are the 5 most effective exercises to help you with your sciatic pain:
Sitting Pigeon Pose:
- Sit on the floor with your legs stretched out straight and your feet together.
- Bend your right leg and cross your right ankle over your left knee.
- Allow the upper body to softly descend toward the thigh as you lean forward at the hips.
- To intensify the stretch, bend the left leg in and place the hands behind the thigh if it is possible without pain or discomfort.
- Hold the stretch for 10–20 seconds, depending on comfort level.
- Slowly release the hold and repeat the stretch on the other side.
Child’s Pose:
- Begin by kneeling and lowering your buttocks onto your heels.
- Knees should be about as far apart as the hips, and the body should be tucked between the thighs.
- Extend the arms in front of the head in a comfortable stance on the floor.
- Relax by taking a few deep breaths into the position.
- Allow the buttocks to rest on the heels rather than forcing them into the posture, resulting in a mild stretch.
- If possible hold the position for 30 seconds.
Leg Bending:
- Lay down on your back and bend your affected side’s knee to 90 degrees.
- While bending and straightening your knee as much as possible without causing pain or other symptoms, keep your foot flexible.
- With no holds, perform 15 reps gently and smoothly. Repeat this process 2–5 times per day.
Knee to Chest:
- Lay on your back
- Bring both knees to your chest.
- Hold 30 to 60 seconds. Repeat 2 -5 times per day.
Bench Lunge:
- Place your affected side’s foot on a chair or a bench.
- In a lunge, rock your hips forth and back while keeping your body upright.
- Rep this action 15-20 times in a steady, rhythmical motion.
How can you book an appointment?
We aim to see you within 24 hours so contact us to make an appointment or to find out more information on how we can help you, please call us on 07515280990 or email us primephysiocareluton@gmail.com. We are one of the best clinics whose physios are registered with HCPC, CSP and Physio first as well have enormous experience.
FAQ’S
Which Physiotherapy is best for sciatica?
Lower back exercises such as extension and flexion relieve pain by promoting movement of the spine. The specific directional movement of the spine usually helps relieve sciatic pain.
Does physio help sciatic nerve?
Yes, By lowering inflammation and relieving muscle tension, physiotherapy treatment has been demonstrated to aid with sciatica pain. The goal is to alleviate sciatica symptoms so you may resume your favourite activities without pain.
How can I strengthen my sciatic nerve?
You can strengthen your sciatic nerve in a number of ways amongst which exercises and stretches are the best option. Pelvic tilt, knee to chest, lower trunk rotations, and all four opposing arm and leg extensions are four sciatica exercises that your spine specialist may offer to assist you relieve sciatic nerve pain and strengthen it.
What exercises should you not do with sciatica?
You should avoid heavy stretching of the hamstrings, straight leg sit ups, bent over rows, full body squats, abdominal stretches, heavy dead-lifts and weight lifting etc.
How do you know when sciatica is healing?
It is as simple as determining whether the pain is “retreating or going” or whether it’s worse. Consider this: if the pain is in your bum one day and your legs the next, the pain has most likely worsened and isn’t getting better. And if the pain is “disappearing,” the sciatica is getting better.