An Eccentric Guide to the Urinary Incontinence
Urinary Incontinence
The uncontrolled leaking of urine is known as urinary incontinence. It signifies that individuals urinate despite their control. The ability to regulate the urinary sphincter is possibly gone or diminished. The condition of urinary incontinence is widespread and affects numerous people. Women suffer incontinence more commonly than men. Compared to 1.5 to 5% of men, it is expected to affect 30% of women between the ages of 30 and 60.
The severity of urinary incontinence can range from occasionally dribbling urine when you sneeze and cough to the instant urge to urinate that doesn’t let you from reaching a restroom in time. Urinary incontinence isn’t a natural part of getting older. Don’t be reluctant to visit a urologist if urinary incontinence interferes with your routine activities. Most people can treat their urinary incontinence symptoms with simple dietary and lifestyle changes or medical attention.
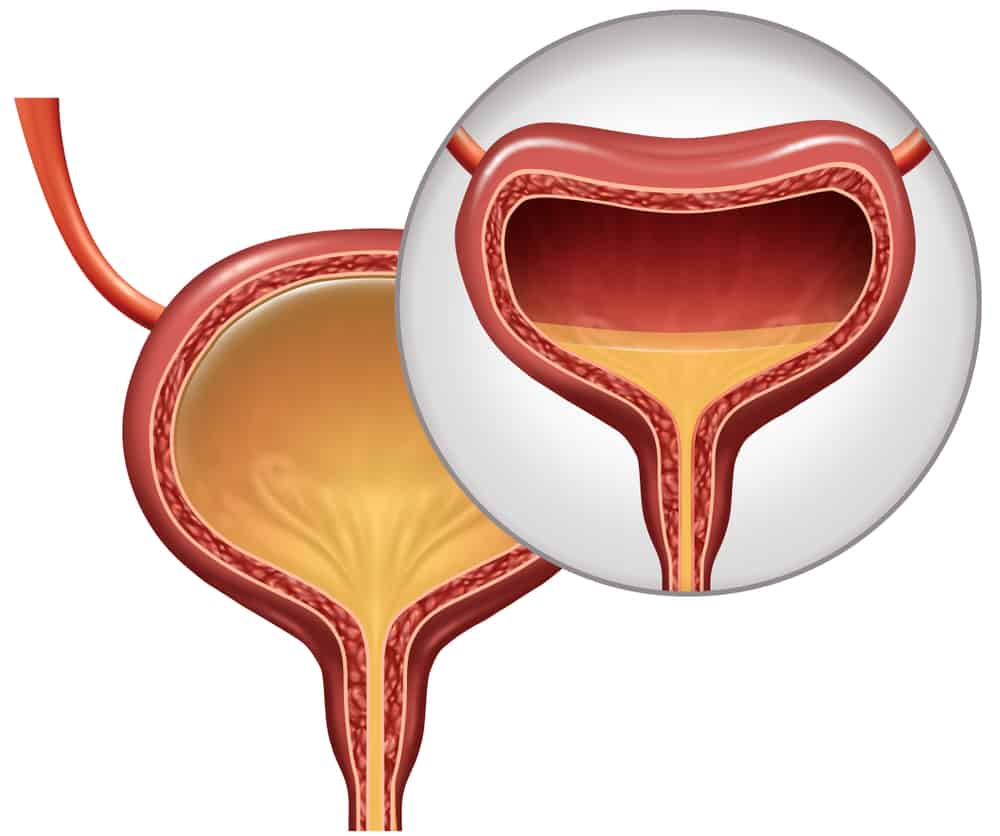
The bladder and the brain manage urinary function. Urine is held in the bladder until you’re ready to empty it. The bladder is kept in position by the muscles in the lower portion of the pelvis. The bladder’s smooth muscles are usually at rest. As a result, the bladder can hold the urine. The bladder’s neck (end) is sealed off. The sphincter muscles enclose the urethra. The tube that takes urine from the body is called the urethra. Urine doesn’t leak when the urethra is kept closed by the sphincter muscles. The brain signals the bladder when you are prepared to urinate. The bladder’s muscles then tighten. In the urethra, the urinal tube is forced to empty. The contraction of the bladder causes the sphincters to open.
Symptoms Of Urinary Incontinence
You can identify the type of urine incontinence based on the urinary incontinence symptoms. Incontinence is not always chronic. Because specific reasons are transient, incontinence will stop when they do. Temporary incontinence may result from vaginal infections. It can be brought on by irritability, medicine, constipation, and limited mobility. Temporary incontinence is also frequently brought on by urinary tract infections (UTIs), which need to be treated.
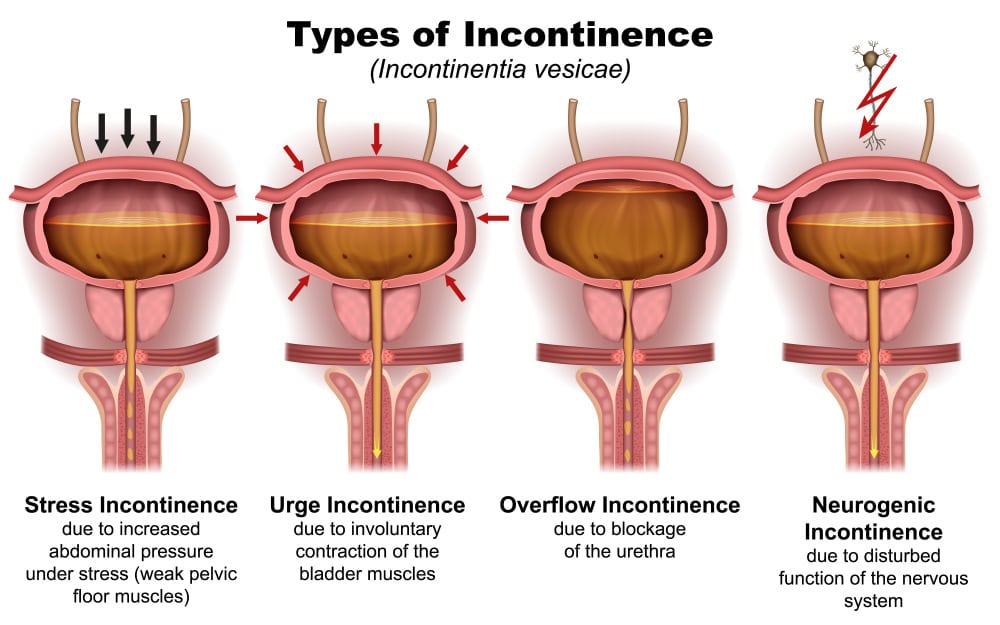
It is crucial to remember that the leakage is likely one of the four categories mentioned above if the cause isn’t transient or straightforward to fix. When urinary incontinence occurs, the pelvic or sphincter muscles (or both) aren’t strong enough to close the bladder and urethra and contain the urine. When you have overactive bladder, the bladder muscles contract excessively, forcing pee out before you’re ready to let it go. Typically, mixed incontinence involves both urinary incontinence and overactive bladder. In overflow incontinence, the bladder fills up past its capacity without emptying.
Types of Urinary Incontinence
Types of Urinary Incontinence
Below we have mentioned the five basic urinary incontinence types:
-
Stress Incontinence
Under this type, urine leaks when you put pressure on your bladder. This condition is known as stress incontinence when unexpected pee leakage is brought on by pressure or abrupt muscular contractions on the bladder. It frequently happens when you exercise, lift heavy objects, cough, sneeze, or laugh. Stress incontinence is the most prevalent issue with bladder control among young and middle-aged women. The problem may develop in younger women due to a pelvic floor muscle deficiency or due to the stress of childbirth. During menopause, stress incontinence in middle-aged women may become a problem.
-
Urge Incontinence
Need incontinence, also known as overactive bladder (OAB), happens when a person experiences an urge to urinate but cannot hold back the urine long enough to reach the restroom. People with a stroke or chronic illnesses, including diabetes, Alzheimer’s disease, Parkinson’s disease, or multiple sclerosis, may occasionally experience urge incontinence. Urge incontinence may sometimes be a precursor to bladder cancer. You have an instant urge to urinate with an uncontrollable loss of urine before reaching the restroom. An infection, a more severe illness like diabetes, or a neurological issue may cause urge incontinence.
-
Functional Incontinence
A physical or mental problem stops you from reaching the restroom quickly. For example, you might be unable to unbutton your jeans quickly enough if you have severe arthritis.
-
Overflow Incontinence
Your bladder doesn’t empty, causing you to urinate excessively or repeatedly.
-
Mixed Incontinence
Having more than one form of urinary incontinence typically means both urge and stress incontinence.
Urinary Incontinence Causes
Urinary incontinence may result from routine behaviors, underlying illnesses, or physical issues. Your doctor can help discover the urinary incontinence causes by completing an evaluation. Drinks, meals, and drugs that stimulate the bladder and increase urine production are known as diuretics.
They include meals and drinks with a lot of spice, sugar, or acid, especially citrus fruits, sedatives, muscle relaxants, high doses of vitamin C, and heart and blood pressure drugs.
Another disorder that is easily managed and may contribute to urinary incontinence is:
-
Urinary Tract Infections
Infections can irritate your bladder, resulting in intense urination desires and, occasionally, incontinence.
-
Constipation
The bladder and the rectum are close neighbors and have many similar nerves. When the hard stool gets stuck in the rectum, these nerves become overactive, which makes people urinate more often.
-
Persistent Urinary Incontinence
Additionally, urinary incontinence may be a chronic disorder brought on by underlying physical issues or modifications, such as:
-
Pregnancy
Stress incontinence can be brought on by hormonal changes and the fetus’s increased weight.
-
Childbirth
A lowered (prolapsed) pelvic floor can result during vaginal delivery, impairing the muscles required for bladder control and harming the bladder neurons and supporting tissue. The bladder or small intestine may protrude into the vagina due to prolapse when forced down from their regular positions. Urinary incontinence may be linked to such protrusions.
-
Age-Related Changes
Bladder muscle aging can reduce the bladder’s ability to hold urine. Additionally, as you age, you experience more frequent involuntary bladder spasms.
-
Enlarged Prostate
In older adults, urinary incontinence is often caused by benign prostatic hyperplasia, an prostate gland enlargement.
-
Prostate Cancer
Men who experience urge or stress incontinence may also have untreated prostate cancer. However, incontinence is more frequently a side effect of prostate cancer therapy.
-
Obstruction
The overflow incontinence can be due to a tumor along the urinary system blocking the usual flow of urine. Urine leakage can occasionally result from urinary stones, which are challenging, stone-like masses that develop in the bladder.
-
Neurological Disorders
Urinary incontinence can be brought on by multiple sclerosis, Parkinson’s disease, or a spinal injury that disrupts the nerve signals that control bladder function.
Medicines for Urge Incontinence
Antimuscarinics
A general practitioner (GP) may prescribe an antimuscarinic drug if bladder training is unsuccessful in managing urge incontinence. Your doctor might also suggest antimuscarinics as a therapeutic option for you if you have overactive bladder syndrome, sometimes called the constant urge to urinate, which can happen with or without urine incontinence. A patch and a pill form of oxybutynin are available, and both should be applied to the skin twice weekly. You can also use the patch; tablets are the most typical delivery technique. A modest dose is frequently used at the start of urinary incontinence treatment to lessen the possibility of side effects. The amount can be increased until the desired result is obtained.
(NOTE: Please consult your physician/GP for personalized medical advice, do not take any medication without consultation. Prime physio Care does not endorse any medications)
Mirabegron
If antimuscarinics do not relieve your incontinence, do not work for you, or cause unfavorable side effects, the doctor may advise you to use a different drug called mirabegron. By relaxing the bladder muscle, mirabegron makes it simpler for the bladder to take in urine and store it. The most popular form is tablets or capsules, usually taken daily.
(NOTE: Please consult your physician/GP for personalized medical advice, do not take any medication without consultation. Prime physio Care does not endorse any medications)
Medicines for Stress Incontinence
After making lifestyle changes or exercising, if stress incontinence does not significantly improve, the next course of action, which is often surgery, will be advised. On the other hand, an antidepressant drug called duloxetine might be helpful for you if you cannot have surgery or would prefer not to. Doing this will likely improve the urethra muscular tone, helping to keep it closed. It would help if you took duloxetine twice daily. After two to four weeks, the doctor will assess your progress to see if the urinary incontinence medication is effective and has any adverse side effects.
(NOTE: Please consult your physician/GP for personalized medical advice, do not take any medication without consultation. Prime physio Care does not endorse any medications)
Elderly Urinary Incontinence Treatment
Below we have discussed urinary incontinence treatment for elderly patients:
Bladder Training
-
Delaying the Event
The objective is to restrain the urge. When the urge to urinate arises, the patient learns how to put it off.
-
Double Voiding
This training entails urinating, waiting a little while, and then urinating again.
-
Toilet Timetable
The person plans to use the restroom at predetermined intervals throughout the day, like every two hours. The patient eventually regains control of their bladder with bladder training.
Surgical Treatment
If alternative treatments do not help, surgery may be a possibility. Before making a choice, pregnant women should examine their surgical decisions with a doctor.
-
Sling Procedures
Under the bladder’s neck, a mesh is placed to stabilize the urethra and prevent urine leakage.
-
Colposuspension
Stress incontinence may be relieved by raising the bladder neck.
-
Artificial Sphincter
An artificial sphincter or valve may be implanted to regulate the urine flow from the bladder into the urethra.
Options Besides
-
Urinary Catheter
A tube that exits the body from the bladder travels via the urethra and empties into a container that holds urine.
-
Absorbent Pads
Shops like pharmacies and supermarkets sell a variety of absorbent pads.
Women’s Urinary Incontinence
The most typical type of incontinence among younger women is stress incontinence. Stress incontinence can happen when the bladder is put under pressure. Weak pelvic floor muscles can bring on stress urinary incontinence causes in females because it makes the bladder and urethra work harder. Other factors that can cause urine leakage include abrupt movements and physical activity.
Urge incontinence is when urine leaks following an urgent desire to urinate before access to a restroom. Some women with urge incontinence must use the restroom more than eight times daily, even if they arrive on time. They don’t urinate regularly whenever they manage to get to the bathroom. Urge incontinence is another word for overactive bladder.
In general, older women are more susceptible to incontinence. It can happen when you least expect it, such as while you’re sleeping, immediately after downing a glass of water, or when you hear or touch flowing water. Urge incontinence affects many women who experience urinary and stress incontinence. These symptoms are a result of mixed incontinence.
Urinary Incontinence in Men
These risk factors could make you more likely to get UI. Several instances of potential risk include:
- In general, older men are a more trustworthy source for user interface design. It could be more difficult to control urination due to physiological changes. The inability to control one’s bladder may be a sign of aging or a symptom of a disease or condition.
- Physical inactivity: While exercise may increase urination frequency, inactivity can result in weight gain and a decline in muscle mass. It might make UTI symptoms worse.
- Obesity: Carrying around the extra weight in the midsection could strain the urinary system.
- You may develop temporary or permanent UI due to treatment for prostate cancer, an enlarged prostate, or either of these conditions. Diabetes can lead to the condition known as insulin resistance (UI).
- Incontinence and other unpleasant symptoms of urinary incontinence in men can result from nervous system disorders that prevent the brain from communicating clearly with the bladder and urinary tract.
The Physiotherapist’s Role in Pelvic Floor Dysfunction
The lower pelvic muscles are impacted by the disorder known as pelvic floor dysfunction. The muscles that surround the pelvic bone and bear the weight of the organs there make up the pelvic floor. Incontinence, difficulty urinating, and the urge to bear down or forward while urinating are symptoms of this illness. Many pelvic floor disorders can benefit significantly from the treatment of a physiotherapist.
Physiotherapy is the initial treatment when a form of pelvic floor dysfunction is identified. Despite the lack of research in this field, some evidence supports the value of physiotherapy. The study has mostly concentrated on the functions that physiotherapists can perform through instruction on dietary changes and exercise recommendations.
A particular form of physical therapy called pelvic floor therapy helps the muscles function and relieves the symptoms of pelvic floor dysfunction. This covers several exercises that support the strengthening and relaxation of your pelvic muscles. A physiotherapist will learn more about your symptoms before you start pelvic floor therapy. Your physiotherapist will examine your core muscles to see their strength and resilience. Additionally, your physiotherapist will ask you to do specific movements and positions to assess how well your pelvic floor muscles work together.
Your evaluation aids your physiotherapist in creating the most effective pelvic floor physical therapy regimen for you. Internal and exterior therapies will likely be used in conjunction during your treatment. However, they won’t start internal treatment until you’re ready because some individuals find it uncomfortable. A physiotherapist’s pelvic floor physical therapy tries to reduce your discomfort and help you get back to your routine. This includes having better bladder control or taking part in activities like sports and exercise that you like. Physical therapy can also help women who experience pain and discomfort during sex. They may find that some workouts improve their orgasms and help them become more conscious of their muscles.
What Can Physiotherapy Do?

Physiotherapy for Urinary Incontinence
Your physiotherapist will design a treatment program to enhance the functionality of your particular pelvic floor muscles. You may be able to regulate your symptoms, use fewer pads, special undies, and medications by following this approach, and you may even be able to avoid surgery. A physiotherapist gives a patient pelvic floor training instructions.
Pelvic Floor Muscle Function Treatments
You’ll learn how to locate (feel the function of) the pelvic floor muscles from your physiotherapist. They will create a workout plan according to your particular condition. By performing these exercises, you may better regulate your bladder and the muscles in your pelvic floor. What might be in your physiotherapy treatment program is:
-
Kegel Exercises
Kegel exercises, also known as pelvic floor contractions, entail contracting the sphincter muscles while pretending to control urine flow. The purpose of the exercise is to cause the muscles to contract and fully relax.
-
Muscle-Strengthening Exercises
You’ll learn specific exercises from your physiotherapist to improve your range of motion, stretch, and muscular strength. Strengthening the pelvic floor muscles supports healthy bladder function.
-
Biofeedback
Your symptoms will determine how you are treated. This alternative will be discussed with you by your physiotherapist. Your physiotherapist will use an inside sensor to read and quantify the activity of the pelvic floor muscles if you feel comfortable beginning this course of treatment. A computer screen will indicate the strain on the probe as you contract your muscles, indicating whether you have squeezed the proper muscles. A physio can guide you via biofeedback, which can also help you become conscious of how to exercise your pelvic floor muscles properly.
-
Electrical Stimulation
Your physiotherapist could use mild electrical stimulation. Your awareness of how your muscles work may improve as a result.
-
Real-Time Ultrasound
To ensure appropriate synchronization, your physiotherapist might use an ultrasound machine to monitor isolated spasms of the abdominal wall and pelvic floor muscles. Additionally, it may help you become more conscious of how your abdominal muscles and pelvic floor work.
Why Go to Physiotherapy?
Despite widespread incontinence is not healthy and can be addressed by a treatment professional, including a physiotherapist. A therapist can assess your issue and assist you in managing urine incontinence using low-risk therapies that can be utilized on their own or in combination with medication and surgical solutions. Ask your doctor to recommend a physiotherapist with specialized training in this field if you believe you could benefit from it. Before referral, a pelvic inspection and urinalysis are highly suggested to detect or rule out conditions that can conflict with or be contraindicated for physiotherapy treatment.
The most effective initial treatment for urine incontinence is physiotherapy. Since the solutions for incontinence in women can be life-changing, we at Prime Physio Care love treating them. During your initial treatment, we will examine your pelvic floor muscles, ask you a few details about your bladder patterns, and explain how the bladder works and how to begin thinking about bladder training. We will require you to fill out a bladder record to evaluate your bladder and urgency, a pelvic ultrasound to evaluate your pelvic floor muscles, and the size, form, and function of your bladder to empty.
How can you book an appointment?
We aim to see you within 24 hours so contact us to make an appointment either online at www.primphysiocare.co.uk or to find out more information on how we can help you, please call us on 07515280990 or email us primephysiocareluton@gmail.com. We are one of the best clinics whose physios are registered with HCPC, CSP and Physio first as well have enormous experience.
Conclusion
In the end, urinary incontinence is a condition that affects many people and significantly impacts their quality of life. Thank goodness, some solutions work. Many women choose not to use these treatments because they feel too ashamed to discuss them.
Most common FAQs
Q: Which four types of urinary incontinence are there?
Incontinence under stress. When you put pressure on your bladder, urine leaks, incontinence caused by an urge, an overflow, or a functional reason
Q: Which drug is the most effective treatment for urinary incontinence?
Anticholinergics: These drugs can help urge incontinence and quiet an overactive bladder.
(NOTE: Please consult your physician/GP for personalized medical advice, do not take any medication without consultation. Prime physio Care does not endorse any medications)
Q: Which natural cure for incontinence works the best?
Kegel exercises are one of the best at-home treatments for urine incontinence. The muscles that stop urine flow are known to be flexed during these workouts. They help treat incontinence in its early stages and gradually strengthen the pelvic floor after surgery.
Q: Is there a cure for urinary incontinence?
The nerves surrounding the bladder that assist in regulating urine and the reflexes of your bladder receive modest electric currents via electrical nerve stimulation. If incontinence is brought on by a shift in the bladder’s position or a blockage by an enlarged prostate, surgery may help reduce or even eliminate it.